Learn More About Our Categories



Caregiver Guidance
Information and tools for getting support, advocating and staying organized.





All Resources
Search for Resources
Clear all filters
Caregiver Guidance
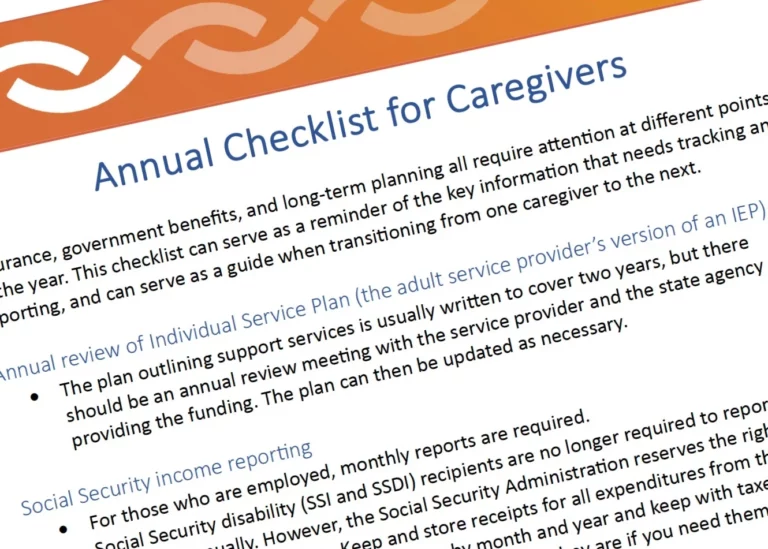
Keeping Important Paperwork Up to Date: A Checklist for Caregivers
Caregiving is a full-time job that includes not just keeping people fed, safe and happy, but making sure that financial, legal and social service supports stay in place.
Insurance, government benefits, and long-term planning all require attention at different points in the year. This checklist can serve as a reminder of the key information that needs tracking and reporting, and can serve as a guide when transitioning from one caregiver to the next.
Annual Review of Individual Service Plan (the Adult Service Provider’s Version of an IEP)
The plan outlining support services is usually written to cover two years, but there should be an annual review meeting with the service provider and the state agency providing the funding. The plan can then be updated as necessary.
Social Security Income Reporting
For those who are employed, monthly reports are required.
Social Security disability (SSI and SSDI) recipients are no longer required to report expenses annually. However, the Social Security Administration reserves the right to audit expenses at any time. Keep and store receipts for all expenditures from the Representative Payee account. Organize by month and year and keep with taxes for at least seven years. This way you know exactly where they are if you need them.
Annual Probate Reports for Guardians (varies by state)
The date for reporting varies from state to state because the laws governing guardianship are different. Often it’s on the anniversary of the date when guardianship was granted by the court.
Many states require a yearly expense report, so it’s helpful to have an organization system for keeping and filing receipts and expenses.
Letter of Intent
A Letter of Intent is a document many families include in their estate plan to help the next generation of caregivers understand the key supports and preferences of the disabled adult. (Learn more about letters of intent from Special Needs Financial Planning).
Everyone’s needs and preferences change over time. Review and update yearly to ensure the Letter of Intent reflects the most recent priorities in the life of the autistic person served by the letter.
Annual Medical Appointments
parent(s)/caregiver(s)
autistic adult
spouses, partners, and siblings, too
annual physical with PCP
dentist
optometrist
gynecologist/urologist
Medication Renewals and Refills
Some prescriptions require a new prescription from a provider on a monthly basis (example: stimulant medications). For many other medications, prescriptions can be written to allow refills for longer periods (up to a year). Schedule in-person visits so that they take place before prescriptions expire.
Open Enrollment for Private Health Insurance
Keep track of enrollment periods, as dates and opportunities vary. Some employers offer open enrollment at the end of the calendar year, while others may offer this window at the beginning or end of a quarter, such as in July or September.
Medicare and Medicaid renewal. Medicare always rolls over at the end of the year. For the most up-to-date information about coverage, contact them directly at 1-800-MEDICARE.
See also our resources on insurance:
Differences Between Medicare and Medicaid
Finding Local Help with Autism Insurance Coverage
Insurance: Turning 26

Communicating About Pain
Autistic people often find that when they feel pain they can’t explain it or locate the source of it as easily as most neurotypical people can.
In the past, some clinicians believed autistic people do not feel pain the way neurotypical people do, which was to say they thought that people who could not verbally communicate about their pain not feeling pain. We now know this isn’t true. Autistic people often find that when they feel pain they can’t explain it or locate the source of it as easily as most neurotypical people can.
Some autistic people may be more sensitive to pain than their neurotypical peers. This can be especially true for girls and women who have autism. This is why talking about pain is one of the most critical conversations to have with a new provider, and it should happen before the first physical exam.
Behaviors that may indicate pain in non-verbal adults
It’s sometimes hard to distinguish between behaviors that indicate pain and those that seek to communicate another problem. Some of the common pain related behaviors are:
Aggression
Running, pacing, bolting
Jumping, stomping, thrashing
Self-injury, sometimes, but not always at the source of the pain (such as banging/hitting head when having GI pain)
Subtle or strong pinching or grabbing body part that source of pain
Sudden, exaggerated repetitive actions, like hand flapping or throat scratching
Twisting or irregular motions/positions to make accommodations for discomfort
Screaming
Ingestion (e.g. overeating, quickly ingesting food and drink, food avoidance, vomiting, mouthing or eating non-food items)
Crying
Withdraws or becomes very still
Checklist for talking to a clinician about pain
It can be helpful to carry a list of pain-related concern to appointments. It might include:
It hurts when people touch me without asking first.
The thought of feeling pain makes me very nervous.
If something will cause pain, please tell me ahead of time.
If something will cause pain, please give me medicine or treatment to help it hurt less.
Pain scares me.
I don’t like needles and need to know if there will be shots or blood draws that might be painful
Using a Pain Scale
If a medical appointment involves addressing pain as a problem or symptom, it may be helpful to use a tool known as a pain scale. Pain scales give patients a way to self-report their pain in a way that helps clinicians make an accurate evaluation and diagnosis of underlying health issues.
There are several kinds of pain scales:
One type of pain scale involves patients assigning a number between 1 and 10 to . One would be “no pain,” and 10 would be the worst pain imaginable.
A non-verbal pain scale for adults may also be used to help communicate about and identify the source and severity of pain. Karen Turner, OT and Patient Navigator at Massachusetts General Hospital, explains:
Karen Turner, OT, is a Patient navigator at the Massachusetts General Hospital in Boston
The Massachusetts General Hospital Patient Accommodations Care Plan is useful communication tool that allows patients and families to document important conditions and behaviors that clinicians should know, including pain.
More information
Neuroscience News on People with Autism Experience Pain at a Higher Intensity
Recent research on autism and pain in adults.
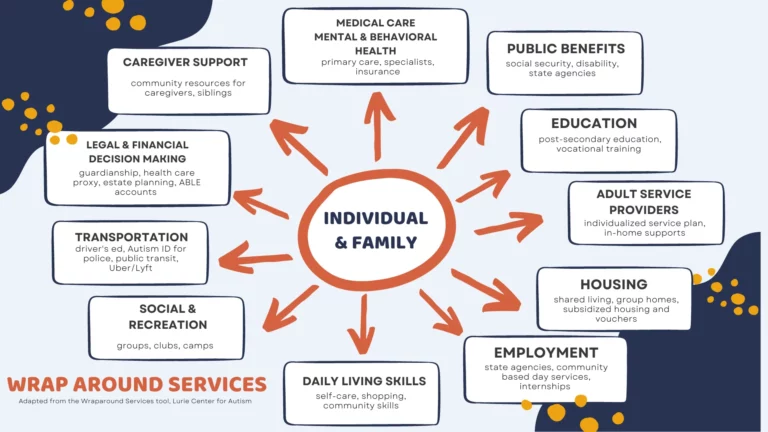
Family Support and Wraparound Services
Many providers have people on staff who can help families understand and navigate a variety of health and community services.
Some medical practices and hospitals have family support clinicians or clinical social workers that can help patients with sensory needs or communication impairments identify support services within the community. Family support clinicians make referrals, collaborate, problem-solve, and connect to supports to help autistic adults and caregivers successfully navigate services across the lifespan. These “wraparound services” address important needs across the lifespan like medical/health concerns, special education, social/behavioral supports, public benefits, legal/financial advice, housing, vocational training, transportation, etc.
Not every medical practice serving adults has a support clinician, but caregivers and self-advocates can encourage the practice to create such a resource. Support clinicians not only improve the lives of autistic adults and their caregivers, but they also ease the workload of the entire practice by ensuring whole-life health for all patients and their caregivers.
Julie M. O’Brien, MEd, LMHC, a Family Support Clinician at the MGH Lurie Center for Autism, helps to educate and support families by identifying a range of home- and community-based supports and resources by age and stage of life. She serves as the liaison between the patients’ provider and parents/guardians/families, and points them in the right direction.
Useful links to find out more about sites and organizations that can help with wraparound services.
Housing
Autism Speaks Resource Guide
Autism Housing Network
Autism Housing Pathways
Education
Postsecondary Education Toolkit
Independent Living and Life Planning
LifeCourse Tools
AANE LifeNet independent Living Support Program
Autistic Self Advocacy Network
Employment
NEXT for Autism
Service Providers
Council of Autism Service Providers
Autism Speaks Directory of Service Providers
Legal & Financial Issues
Autism Advocacy Law Center
Guide for a Letter of Intent
Financial Planning Toolkit
Social Connections & Supports
AANE Online Support and Discussions
Support for Families of Those with Profound Autism
Profound Autism Alliance

How is Autism Different in Women?
Autism is a diverse condition that affects individuals of all genders. Although it is still more commonly diagnosed in males, recent research suggests that the disparity is shrinking as awareness of how autism presents in females increases.
This article is based on a LurieNOW article by Dr. Alyssa Milot Travers, a licensed psychologist at the Lurie Center for Autism with specific expertise in women on the autism spectrum. Dr. Travers is also an Instructor in Psychiatry at Harvard Medical School.
Autism is a diverse condition that affects individuals of all genders; the overall prevalence estimate of autism in the U.S. is one in 36 children. According to the Centers for Disease Control and Prevention (CDC), as of March 2023 about 4% of boys and 1% of girls age 8 years have autism.
Although an autism diagnosis occurs more often in men than in women, recent research suggests that autism in women may be both underdiagnosed and misdiagnosed. Recognizing and understanding how autism presents in women is crucial for accurate diagnosis, appropriate support, and targeted interventions. The evolving understanding of gender differences in autism is dismantling the notion that autism is more or less a “male condition.”
Gender identity in autism research
The majority of autism research in recent decades has focused on cisgender individuals, or those who have a gender identity that matches their sex assigned at birth. The most current research reveals that gender diversity is more common in autistic people than in their neurotypical peers. Consequently, there is a slow but distinct shift toward including gender diversity in autism research, which will provide a more accurate representation of all autistic individuals. The current knowledge of the female subtype of ASD is based on research of cisgender women.
Outward signs: Special interests and repetitive behaviors
Restricted interests and repetitive behaviors occur in autistic men and women; however, the nature of these behaviors can differ. Traditionally, clinicians have been trained to recognize stereotypical male-associated restricted interests, such as transportation, dinosaurs, or space. In contrast, autistic women may develop interests that are more closely aligned with societal norms, such as animals, art, celebrities, or literature.
This divergence can contribute to the misconception that women with these types of restricted interests are simply displaying enthusiastic hobbies rather than autistic traits. Repetitive patterns of behavior in women may manifest as classic autistic behaviors like rocking or hand/finger movements. However, they may also appear as behaviors not necessarily associated with autism, such as perfectionistic tendencies or restrictive patterns of eating/eating disorders.
Impediments to an ASD diagnosis: Overshadowing, masking, and camouflaging
Based on behavioral history, women may be more apt to receive diagnoses such as anxiety, mood disorders, learning disorders, and/or eating disorders rather than autism. This phenomenon is called diagnostic overshadowing, which occurs when a person’s symptoms are attributed to a psychiatric problem versus an underlying medical condition or a developmental delay such as autism. This can complicate the diagnostic process, as the focus may be on managing these secondary conditions rather than recognizing the underlying autistic traits.
Autistic women are also more likely to develop compensatory strategies to mask their challenges. For example, women often have stronger social imitation skills and the ability to mimic social behavior compared to men. Due to their social foundation, girls may develop one or two close friendships, helping them absorb social rules and norms. Their strong social interest may lead them to “camouflage” or compensate for social understanding and communication challenges, making these vulnerabilities difficult to detect in everyday interactions or larger classroom or employment settings. As a result of these differences, women are often more likely to be diagnosed later in life, if at all.
The Autistic Women and Nonbinary Network provides useful information and resources for gender-diverse autistic individuals.
For diagnostic resources, see our article about seeking an ASD diagnosis as an adult.
Recommended Reading and Viewing
For women:
Camouflage: The Hidden Lives of Autistic Women by Dr. Sarah Bargiela
22 Things a Woman with Asperger’s Syndrome Wants Her Partner to Know by Rudy Simone
The Autistic Brain: Exploring the Strengths of a Different Kind of Mind by Temple Grandin
Odd Girl Out: An Autistic Woman in a Neurotypical World by Laura James
From the American Autism Association: 5 TedX Talks from Women with Autism
For caregivers:
A Guide to Mental Health Issues in Girls and Young Women on the Autism Spectrum: Diagnosis, Intervention and Family Support by Dr. Judy Eaton
Girls Growing Up on the Autism Spectrum: What Parents and Professionals Should Know About the Pre-Teen and Teenage Years by Shana Nichols with Gina Marie Moravcik and Samara Pulver Tetenbaum
For partners of autistic adults:
The Other Half of Asperger Syndrome: A Guide to Living in an Intimate Relationship with a Partner Who is on the Autism Spectrum by Maxine Aston

Autism and Grief
The transitions surrounding loss are some of the most unrecognized and difficult ones for autistic people. Like many deeply emotional events, autistic people often process the separation differently.
Processing loss
The transitions surrounding loss are some of the most unrecognized and difficult ones for autistic people. Like many deeply emotional events, autistic people often process the separation differently. At the same time, many autistic people take comfort from the rituals that accompany death in many cultures. Events such as wakes, funerals, memorial services, and burials can be helpful transition points that acknowledge loss and give it context. Even for those who cannot or choose not to participate fully, these events can encourage conversations about the person who has died. For more advice and ideas, including information about how many religions address death, visit the award-winning Autism and Grief Project.
Signs of grieving
Autistic people may not react to loss or express grief in real time. A delayed reaction might appear week or months later and take the form of:
unusual behavior changes such as dysregulation, mood swings, and aggression
social and emotional withdrawal
spurts in stereotypy or repetitive behaviors
increases in creative activities such as drawing, painting, or collecting.
Coping with loss
One of the biggest challenges that can come with loss is the change in routine. When it’s possible to plan for the grieving process, it can be helpful to update or create new routines that can replace or fill the inevitable void. It’s also useful to remember that everyday tasks can take on added meaning when done with or for someone beloved. Creative ways for an autistic adult to help remember a loved one can include:
designing printed memorial cards
creating one or more photo and/or memory books (a portable one that can be carried in a backpack or the car can be helpful when away from home)
assembling a slide show that can be watched on a phone or tablet
creating a drawing or collage, or establishing a routine around making these types of art projects
establishing a dedicated place to collect and display mementos that recall positive memories
recreating fond food memories by making or eating special meals.
Author Susan Senator, parent of an autistic adult, has advice about How to Help an Autistic Person Process Grief and Loss in Psychology Today.
Losing our beloved Poppa was traumatic, and he insisted that he did not want a funeral. The lack of closure was very difficult for our autistic adult son, who misinterpreted the wish for no formal services as a sign that his grandfather died from a broken heart. He would talk of little else for months, until we set aside times together to spread some ashes in a few of his Poppa’s favorite places.
— Sarah T., parent of an autistic adult

The Formal Diagnostic Criteria for Autism
When a clinician makes a formal diagnosis of Autism Spectrum Disorder, they use the criteria laid out in the Statistical Manual of Mental Disorders, Volume V, 2013. It reads as...
When a clinician makes a formal diagnosis of Autism Spectrum Disorder, they use the criteria laid out in the Statistical Manual of Mental Disorders, Volume V, 2013.
It reads as follows:
Autism Spectrum Disorder
Diagnostic Criteria 299.00 (F84.0)
Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive; see text):
Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions.
Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication.
Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts; to difficulties in sharing imaginative play or making friends; to absence of interest in peers.
Specify current severity: Severity is based on social communication impairments and restricted, repetitive patterns of behavior (see Table below).
Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text):
Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases).
Insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat same food every day).
Highly restricted, fixated interests that are abnormal in intensity or focus (e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interests).
Hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement).
Specify current severity: Severity is based on social communication impairments and restricted, repetitive patterns of behavior (see Table below).
Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learned strategies in later life).
Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
These disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and autism spectrum disorder frequently co-occur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level.
Note: Individuals with a well-established DSM-IV diagnosis of autistic disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified should be given the diagnosis of autism spectrum disorder. Individuals who have marked deficits in social communication, but whose symptoms do not otherwise meet criteria for autism spectrum disorder, should be evaluated for social (pragmatic) communication disorder.
Specify if: With or without accompanying intellectual impairment
With or without accompanying language impairment
Associated with a known medical or genetic condition or environmental factor (Coding note: Use additional code[s] to identify the associated medical or genetic condition.)
Associated with another neurodevelopmental, mental, or behavioral disorder (Coding note: Use additional code[s] to identify the associated neurodevelopmental, mental, or behavioral disorder[s].)
With catatonia (refer to the criteria for catatonia associated with another mental disorder, pp. 119-120, for definition) (Coding note: Use additional code 293.89 [F06.1] catatonia associated with autism spectrum disorder to indicate the presence of co-morbid catatonia.)
Social (Pragmatic) Communication Disorder
Diagnostic Criteria 315.39 (F80-.89)
Persistent difficulties in the social use of verbal and nonverbal communication as manifested by all of the following:
Deficits in using communication for social purposes, such as greeting and sharing information, in a manger that is appropriate for the social context.
Impairment of the ability to change communication to match context or the needs of the listener, such as speaking differently in a classroom than on a playground, talking differently to a child than to an adult, and avoiding use of overly formal language.
Difficulties following rules for conversation and storytelling, such as taking turns in conversation, rephrasing when misunderstood, and knowing how to use verbal and nonverbal signals to regulate interaction.
Difficulties understanding what is not explicitly stated (e.g., making inferences) and nonliteral or ambiguous meanings of language (e.g., idioms, humor, metaphors, multiple meanings that depend on the context for interpretation).
The deficits result in functional limitations in effective communication, social participation, social relationships, academic achievement, or occupational performance, individually or in combination.
The onset of the symptoms is in the early developmental period (but deficits may not become fully manifest until social communication demands exceed limited capacities).
The symptoms are not attributable to another medical or neurological condition or to low abilities in the domains of word structure and grammar, and not better explained by autism spectrum disorder, intellectual disability (intellectual developmental disorder), global development delay, or another mental disorder.
Reprinted with permission from American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Copyright © 2013. American Psychiatric Association. All Rights Reserved. Permission from the APA is required to reproduce DSM-5 Criteria and any Related Tables.
More information from AAHR
Getting an Autism Diagnosis as an Adult
The Language of Autism
How is Autism Different in Women?

Sibling Relationships
Communication is key to building healthy relationships and smooth transitions among family members.
Brothers and sisters, or siblings, are often key players for autistic adults and their caregivers, especially during transitional times. Research shows that autistic people who have siblings develop better social skills as well as a built-in resilience.
If an autistic person has more than one sibling, they are likely to have a different relationship with each. For example, some siblings may be able to provide strong emotional support, while others may be better at helping with, or taking on, decisions about finances and care. These roles can evolve across the lifespan, so it’s important that siblings try and maintain positive communication — not only with the autistic adult, but with one another.
Unique family dynamics
As in any family, sibling relationships change over time, but there can be unique challenges for both the autistic adult and their siblings during different stages of life. For example, older siblings might feel a sense of responsibility toward their autistic sibling and feel tentative about building a life outside the family unit. Younger siblings gain independence and develop skills and relationships that lead them to surpass their older, developmentally delayed autistic sibling. When this happens, autistic adults may struggle with feeling abandoned or jealous when a younger sibling moves out, gets married, or has children, while siblings in turn can feel guilty about becoming more independent.
Navigating sibling milestones
The goal for caregivers is to encourage the autistic adult to accept and adapt to the changes in routine and family structures, to ensure that siblings feel empowered to build independent lives while maintaining family connections. It’s productive to have conversations with the autistic adult about sibling life milestones in advance, to the extent that it’s possible. For example, when siblings prepare to leave home, caregivers can address:
how daily routines will change
when siblings will come home or when family will visit them
whether a sibling’s space or room will stay the same or be used for something else
ways siblings can communicate regularly (email, letter, video call).
Caregivers can help siblings by encouraging and supporting their life choices outside of the family home and communicating regularly about any changes in care, employment supports, and living arrangements with their autistic sibling. Keeping siblings informed about specific and general caregiver responsibilities gives them a chance to consider what role they may feel comfortable playing during their autistic sibling’s later years.
Resources for siblings
As attuned as caregivers can be to the needs of all of their children, parents who did not grow up with an autistic sibling can’t always empathize or understand the impact of autism on siblings. For most siblings, autism has punctuated their entire childhood. Siblings often benefit from talking with other siblings of autistic people or speaking with a therapist familiar with the dynamics of families touched by autism.
Because anxiety and depression are more common among siblings of autistic people, it’s important to assure that support and care are readily available. For families of people whose autism includes challenging behaviors, Autism Speaks has a guide for siblings and a Q&A that addresses some of those issues.
Sibling roles as caregivers age
Just as setting expectations and arranging for visits and regular contact is key when siblings first leave home, communication becomes increasingly important as caregivers and autistic adults get older. Family gatherings and holidays can be stressful for siblings if it is assumed they will replicate childhood rituals or vacation in the same place every year. Siblings can assist in skillfully introducing new activities alongside longtime family traditions, which serves to lighten the load on caregivers and prepare for transitions of care.
Another key consideration for siblings is how to plan for the time when parents, caregivers, or guardians can no longer provide care or support for the autistic adult. This is especially challenging when an autistic adult still lives at home. Siblings need to understand what caregivers do day-to-day long before this transition occurs, so that they are prepared to make decisions about care and support when the time comes.
Some things to consider:
How well do the siblings get along with their autistic sibling?
How do the neurotypical siblings get along with each other?
Have siblings been made aware of financial arrangements for their autistic sibling?
Are siblings prepared to advocate for the autistic adult?
Do siblings understand the medical needs of the autistic adult?
Caregivers can create opportunities to discuss and answer these questions and incorporate them into plans as they approach later transitions.
Learn more
AAHR article on Family Support and Wraparound Services
The Profound Autism Alliance has a Sibling Action Network
Autism Speaks: A Sibling’s Guide to Autism
Autism Speaks Q&A: Supporting Siblings of Autistic Children with Aggressive Behaviors
How to Bring Adult Siblings Into an Autistic Brother’s Life by Susan Senator in Psychology Today
The Sibling Support Project has resources and trainings for siblings of people with developmental disabilities
Autism Spectrum News on Adult Sibling Support
The Autism Science Foundation has a site with multiple resources for siblings, Sam’s Sibs Stick Together
Navigating Grief and Loss: A Guide for Siblings of people with IDD
Next steps: Starting the Conversation: Future Planning and Siblings of People with IDD.

Types of Mental Health Providers
When seeking mental health care - therapy, diagnoses or medication - it's helpful to know which providers offer which kinds of care.
Psychiatrists are licensed physicians (MDs or DOs) that evaluate and diagnose mental health conditions, prescribe and monitor medications, and provide therapy.
Psychiatric or mental health nurse practitioners evaluate and diagnose mental health conditions, prescribe and monitor medications, and provide therapy. Similar to a psychiatrist, they are also qualified to prescribe and monitor medications (regulations vary by state).
Psychiatriatric pharmacists/psychopharmacologist (PharmD) are advanced-practice pharmacists who specialize in mental health care, including prescribing and monitoring medications.
Psychologists can evaluate and diagnose mental health conditions, assess patients’ mental states, emotional processes, and behavior, and provide therapy. Clinical psychologists with specialized training can also complete more detailed psychological and neuropsychological assessments.
Clinical neuropsychologists (PhD) are clinical psychologists with specialized training who conduct detailed neuropsychological evaluations, including assessment of general intellectual abilities, language, attention, memory, motor skills, and emotional and behavioral functioning.
Licensed professional counselors (LPCs) are licensed mental health counselors who provide mental health and substance use care.
Licensed marriage and family therapist (LMFTs) are licensed to evaluate, diagnose, and treat mental and emotional disorders within the context of marriage, couples, and family systems.
Licensed clinical alcohol & drug abuse counselors (LCADACs) provide substance use counseling and diagnosis, prevent, treat, and ameliorate psychological problems, emotional conditions, or mental conditions of individuals or groups.
Clinical social workers (MSW) provide a range of social work services, including treatment for mental illnesses.
Licensed clinical social workers (LCSWs) are licensed clinical social workers who can evaluate, diagnose, and treat patients’ mental, emotional, and behavioral disorders under the continued clinical supervision of an LICSW.
Licensed independent clinical social workers (LICSWs) are licensed professionals who independently practice clinical social work, including the ability to evaluate, diagnose, and treat patients’ mental, emotional, and behavioral disorders. LICSWs work to restore or enhance patients’ social and psychosocial functioning.
More information:
The National Alliance for Mental Illness (NAMI) offers help finding mental health providers and links to support groups.
The Substance Abuse and Mental Health Services Administration offers 24-hour referral and support.
SAMHSA’s National Helpline800-662-HELP (4357)TTY: 800-487-4889
All talk of and thoughts about suicide are serious.
People facing a mental health crisis or thoughts of suicide can call or text 988 from any phone.
For more help and information contact Lifeline.
Deaf and hard of hearing adults can access 988 resources by using the “ASL now” button on the 988 Lifeline site, or by dialing 800-973-8255 with a phone capable of making video calls
Clinical Care for Autistic Adults
Clinical Care for Autistic Adults is led by nationally recognized experts, with extensive expertise caring for adults with autism.
A course for medical professionals
Given the unique needs of autistic adults, many clinicians find themselves underprepared for the complexity of diagnoses, the diversity of presentations, and the coordination of care. Clinical Care for Autistic Adults is led by nationally recognized experts, with extensive expertise caring for adults with autism.
Clinical Care for Autistic Adults is designed for clinicians who currently provide care to autistic adults or are preparing to welcome autistic patients into their practice. Its goal is to empower clinicians to provide personalized care for autistic people and their families. Clinicians who complete this course will able to:
Recognize the range of needs that autism presents across spectrum and age
Examine the gaps that exists for support of adult autistic patients
Identify key players in the ongoing support of autistic patients throughout the adult lifespan
Apply best practices and strategies to better support patients during adult primary and specialist visits, screenings, and medical procedures
Develop and utilize communication protocols to increase effectiveness of transitions of care
See the course description: Clinical Care for Autistic Adults
Share this code with providers to give them direct access to the course:

Medical Facilities for After-Hours Care
Health care problems often arise outside of primary care physican’s (PCP) regular office hours. It’s good to know what other options are available for medical care if you become sick or injured with a non-life-threatening condition after hours or if you’re traveling away from home.
When health care problems arise at night, on weekends, or away from home, it’s good to know what the options available for after-hours medical care. The first step is to call your primary care physician’s (PCP) office. They will likely have instructions on their voicemail or their answering service will connect you to a clinician on call.
If you choose to, or are directed to care at an outside medical facility, it is helpful to have a clear idea about what a particular facility can or cannot treat. When possible, call ahead to find information about scope of services, hours, potential wait time, and types of insurance accepted. Some walk-in clinics and urgent care facilities have online appointment and check-in procedures that allow patients to make appointments for the best or first-available time. Be sure to bring an Emergency Go Bag for extended or unexpected wait times.
It’s also helpful to understand the distinction between the scope of care and types of providers that a walk-in or urgent care center may offer in comparison to an emergency department. Depending on state requirements, for example, a walk-in clinic or an urgent care center may not necessarily have physicians, mental health clinicians, or radiologists on site.
Types of medical care facilities outside of a PCP office
Walk-in clinic. Provides non-urgent/non-emergency basic medical care for minor conditions such as colds, flu, cuts, or skin conditions. Many urgent care centers (see below) take walk-ins.
Urgent care center. A step up in care from a typical walk-in clinic, urgent care centers also treat non-urgent/non-emergency illnesses or injuries along with conditions that may require laboratory and x-ray services.
If a health care problem is determined to be a true medical emergency, the walk-in or urgent care staff will refer the patient to an emergency department. Transfer by ambulance will be assessed depending on the urgency of the situation.
Emergency department (ED) (often called emergency room). The designated part of the hospital that provides unscheduled, 24/7 care for serious illnesses, accidents, or mental health crises. EDs stabilize and treat patients with medical emergencies. If further care is required, then a patient may be admitted to the hospital.

Planning for Medical Emergencies
Everyone—autistic people and neurotypical people—can benefit from planning for medical or mental health emergencies.
Be ready: Make a 'Go Bag'
Emergencies are easier to handle if information and supplies are at the ready. Keeping a Go Bag near the door or in the car can help.
The Go Bag – a printable list of things to have on hand to help prepare for emergencies
Start by calling the PCP
Everyone—autistic people and neurotypical people—can benefit from planning for medical or mental health emergencies. If a trip to the emergency department (ED) is necessary, you’ll want to alert your primary care provider’s office (another person in the household can make this call as necessary). It’s especially helpful to request that the PCP call ahead and let the ED or hospital know that an autistic patient is on the way and they can share any pertinent information that can be helpful for your care.
Make a call tree
Another key part of the plan is to create a call tree that includes someone in the circle of support who can contact others who should be alerted to the emergency. This information should be clearly displayed in a prominent position in your home. This is especially important for first responders-police, fire, and EMS – in case you are alone during an emergency. The call tree contacts can include service provider or group home staff, neighbors who can assist with caring for others in the family, and extended family.
Register with the local police
Most local police departmetns have a way of registering citizens with special health needs. If there are details they should know about how autism presents in you or the adult in your family take a moment to communicate about those concerns. For example, some people panic and hide when they hear sirens, see someone in uniform, or even hear the doorbell.
Calling 911
Most clinicians’ offices direct people in crisis to the local emergency department or urgent care center. If calling 911 is the best or only option, clearly state to the dispatcher that the patient is a person with autism and let them know about any communication or behavioral challenges that might be misunderstood. Many first responders are trained to interact with autistic people but many are not – it’s important to know ahead if time if local police, fire, and EMS are trained in working with the autistic community. Autism Speaks has a guide for first responders that can be shared with local public safety organizations, including information for dispatchers. In addition, there are several programs that train first responders to safely interact with autistic people, including Autism Alert and Autism Risk and Safety Management.
Tips for interacting with first responders
Whether an emergency occurs in the home or out in the community, an autism ID can be useful. It can be a simple card with details that are specific to the individual and can help avoid misunderstandings in stressful situations. Caregivers can share an ID card or self-advocates can carry them and share as necessary.
The card be shared with first responders or with staff and clinicians in emergency departments, urgent care, and hospitals. There are Medicalert IDs for autism and also sites that can create an autism ID for a fee. This one was created using a free site called Canva:
A sample identification card that outlines what strategies autstic people can use to communicate in an emergency
Mental health emergencies
When there’s a mental health emergency, think carefully about what the goal is for taking someone to the Emergency Department. Dr. Robyn Thom, a psychiatrist at the MGH Lurie Center for Autism, discusses expectations for a mental health care visit to the Emergency Department:
Dr. Robyn Thom on things to consider when going to the emergency room for a mental health emergency.
A 3×5 identification card to print and use for communicating in an emergency

Medical Specialists and What They Treat
Many autistic adults and caregivers are familiar with the type of medical care that specialists, such as neurologists and gastroenterologists, provide for co-occuring health conditions. We’ve compiled this list of specialists so that autistic adults are familiar with more types of clinicians that treat health issues that may arise across the lifespan.
Allergists or immunologists treat allergies, asthma, and immunologic disorders, including primary immunodeficiencies.
Anesthesiologists administer anesthetics and analgesics for pain management pre-, during, and post-surgical procedures.
Cardiologists treat conditions related to the cardiovascular system (heart and blood vessels).
Dermatologists treat conditions related to the skin, hair, and nails.
Endocrinologists treat hormone-related conditions.
Gastroenterologists treat conditions related to the digestive system.
Geriatric physicians/geriatricians treat medical and psychological conditions associated with aging.
Hematologists treat blood disorders, including leukemia.
Infectious disease specialists treat conditions related to infections that are contagious.
Nephrologists treat conditions related to kidney function.
Neurologists treat conditions affecting the nervous system (brain, nerves, and spine).
Medical geneticists diagnose and treat genetic (inherited) conditions.
Obstetrician/gynecologists (OB/GYNs) treat conditions related to female reproductive health, including pregnancy, childbirth, menstruation, and menopause.
Oncologists specialize in diagnosing and treating cancer.
Ophthalmologists treat conditions related to the eyes.
Otolaryngologists or “ear, nose, and throat” clinicians (ENTs) treats conditions involving the throat, tonsils, sinuses ears, mouth, head, and neck.
Podiatrists treat conditions affecting feet, ankles, and related structure of the legs.
Proctologists or colorectal surgeons specialize in diseases and conditions of the lower digestive tract, including the anus, colon, and rectum.
Pulmonologists treat conditions related to breathing functions of the lungs and heart.
Rheumatologists treat rheumatic and autoimmune conditions affecting the bones, joints, tendons, and muscles.
Urologists treat conditions of the urinary tract and also care for male reproductive health.
For a more comprehensive list of specialists go to the HHP List of specialists.
Allergists or immunologists treat allergies, asthma, and immunologic disorders, including primary immunodeficiencies.
Anesthesiologists administer anesthetics and analgesics for pain management pre-, during, and post-surgical procedures.
Cardiologists treat conditions related to the cardiovascular system (heart and blood vessels).
Dermatologists treat conditions related to the skin, hair, and nails.
Endocrinologists treat hormone-related conditions.
Gastroenterologists treat conditions related to the digestive system.
Geriatric physicians/geriatricians treat medical and psychological conditions associated with aging.
Hematologists treat blood disorders, including leukemia.
Infectious disease specialists treat conditions related to infections that are contagious.
Nephrologists treat conditions related to kidney function.
Neurologists treat conditions affecting the nervous system (brain, nerves, and spine).
Medical geneticists diagnose and treat genetic (inherited) conditions.
Obstetrician/gynecologists (OB/GYNs) treat conditions related to female reproductive health, including pregnancy, childbirth, menstruation, and menopause.
Oncologists specialize in diagnosing and treating cancer.
Ophthalmologists treat conditions related to the eyes.
Otolaryngologists or “ear, nose, and throat” clinicians (ENTs) treats conditions involving the throat, tonsils, sinuses ears, mouth, head, and neck.
Podiatrists treat conditions affecting feet, ankles, and related structure of the legs.
Proctologists or colorectal surgeons specialize in diseases and conditions of the lower digestive tract, including the anus, colon, and rectum.
Pulmonologists treat conditions related to breathing functions of the lungs and heart.
Rheumatologists treat rheumatic and autoimmune conditions affecting the bones, joints, tendons, and muscles.
Urologists treat conditions of the urinary tract and also care for male reproductive health.
For a more comprehensive list of specialists go to the HHP List of specialists.

Types of Primary Care Providers
Primary Care Providers (PCPs) are often the first to diagnose and treat medical problems that affect adults. They also identify risk factors for disease and offer advice on prevention.
Primary care providers (PCP) provide health care on an as-needed and long-term basis for people in early adulthood through older age. PCPs are often the first to diagnose and treat medical problems that affect adults. They also identify risk factors for disease and offer advice on prevention. General services that primary care clinicians provide include:
perform age-appropriate periodic wellness assessments
prescribe medications
treat illnesses and injuries
screen for common health issues based on personal risk factors and family history
manage acute and chronic conditions
order diagnostic tests
make referrals to specialty clinicians when necessary
A PCP may be one of the following types:
Medical Doctors (MD) or Doctors of Osteopathy (DO) may also be called Internal Medicine Doctors.
Nurse Practitioners (NP) provide primary care independently or in conjunction with/under supervision of a physician (varies depending on state regulations).
Family Practice physicians can treat all age ranges within a family, asservices include pediatric and OB/GYN care.
Supporting health care professionals that provide care under the supervision of MD, DO, or NP:
Physician Assistants (PA) are licensed medical professionals that provide many of the same services as primary care physicians. PAs can examine, diagnose, and treat patients and are able to assist in minor procedures. PAs are also able to prescribe medications.
Nurses (RN, LPN, APRN) assist PCPs by delivering specified types of patient care and implementing treatment plans such as administering medications. Nurses are unable to prescribe medications.
Medical Assistant (MA) complete both administrative and clinical tasks in hospitals, physician offices, and other healthcare facilities. Their tasks can include taking medicals histories, preparing patients for examinations, and explaining procedures.
More information is available from the American Academy of Family Physicians.

Guardianship for Autistic Adults
Some people with autism make their own health care and medical decisions. Others cannot or prefer to have someone help them with these decisions. When health care matters are complex...
Some people with autism make their own health care and medical decisions. Others cannot or prefer to have someone help them with these decisions. When health care matters are complex or overwhelming it might be necessary to appoint a guardian. A health care guardian has the legal right to make health care decisions for another person, with full permission to access records and communicate with providers. A health care guardian may also be called a medical guardian.
Who should consider a health care guardian?
Caregivers for people with autism who interact with their clinicians are often required to become guardians so that they can do things like make appointments, access medical records and make important decisions in an emergency. A family with an autistic person should consider guardianship if there’s difficulty with at least one area of life:
Health care: The person cannot understand, communicate and decide about their own health care.
Food and shelter: The person cannot manage money, provide their own food or place to live.
Potential for exploitation, serious injury or illness: The person cannot consistently make decisions that help them stay safe.
Whenever possible, guardians are obligated to give their autistic family member a chance to understand and weigh in on all decisions.
Lisa Nowinsky, PhD, title, discusses guardianship and medical decision making for autistic adults:
Lisa Nowinski, PhD, Director of Non-Clinician Service, MGH Lurie Center for Autism
Health care guardians and other options for autistic adults
There are several options to consider when it comes to seeking guidance for medical decision-making. They may:
Request permission for someone to see their medical information and help with decisions.
Patients must give written permission for a family member to see their health information or help with decisions. Doctors have medical release forms in their offices or on their patient portals.
Use a tool called Supported Decision Making.Supported Decision Making is a way of seeking help with complex medical decisions. The final decision lies with the patient, but they can bring other people (family, friends, support professionals, or other clinicians on their care team) into the conversation so that they make an informed choice.
Self-advocates who do not need a guardian can learn more about the kinds of support they can get from the American Civil Liberties Union’s FAQs on Supported Decision-Making.
Full guardianship.Guardianship is a legal process that often requires a lawyer, and each state has its own rules and may even have different types of guardians – it’s important to review the criteria for the state in which the autistic person lives. Legal forms are available at state government websites.
An attorney at Autism Spectrum News provides more details: Legal Guardianship: The Pros and Cons for Your Adult Disabled Child
Once guardianship is established, there are requirements for keeping it in place, usually an annual report filed in probate court (no lawyer required for that). Guardians should have proof of guardianship with them at all medical appointments and anywhere medical decisions are made. It’s a good idea to keep a copy of proof of guardianship (usually the court document awarding guardianship) in the car, backpack or purse.
Up for discussion
Guardianship decisions and the rules governing them are under review in many states as autistic self-advocates raise concerns about their right to make their own decisions. The National Council on Disability’s report Turning Rights into Reality: How Guardianship and Alternatives Impact the Autonomy of People with Intellectual and Developmental Disabilities provides useful information about the changing attitudes and legislative initiatives affecting guardianship.
Communication Strategies

Communicating About Pain
Autistic people often find that when they feel pain they can’t explain it or locate the source of it as easily as most neurotypical people can.
In the past, some clinicians believed autistic people do not feel pain the way neurotypical people do, which was to say they thought that people who could not verbally communicate about their pain not feeling pain. We now know this isn’t true. Autistic people often find that when they feel pain they can’t explain it or locate the source of it as easily as most neurotypical people can.
Some autistic people may be more sensitive to pain than their neurotypical peers. This can be especially true for girls and women who have autism. This is why talking about pain is one of the most critical conversations to have with a new provider, and it should happen before the first physical exam.
Behaviors that may indicate pain in non-verbal adults
It’s sometimes hard to distinguish between behaviors that indicate pain and those that seek to communicate another problem. Some of the common pain related behaviors are:
Aggression
Running, pacing, bolting
Jumping, stomping, thrashing
Self-injury, sometimes, but not always at the source of the pain (such as banging/hitting head when having GI pain)
Subtle or strong pinching or grabbing body part that source of pain
Sudden, exaggerated repetitive actions, like hand flapping or throat scratching
Twisting or irregular motions/positions to make accommodations for discomfort
Screaming
Ingestion (e.g. overeating, quickly ingesting food and drink, food avoidance, vomiting, mouthing or eating non-food items)
Crying
Withdraws or becomes very still
Checklist for talking to a clinician about pain
It can be helpful to carry a list of pain-related concern to appointments. It might include:
It hurts when people touch me without asking first.
The thought of feeling pain makes me very nervous.
If something will cause pain, please tell me ahead of time.
If something will cause pain, please give me medicine or treatment to help it hurt less.
Pain scares me.
I don’t like needles and need to know if there will be shots or blood draws that might be painful
Using a Pain Scale
If a medical appointment involves addressing pain as a problem or symptom, it may be helpful to use a tool known as a pain scale. Pain scales give patients a way to self-report their pain in a way that helps clinicians make an accurate evaluation and diagnosis of underlying health issues.
There are several kinds of pain scales:
One type of pain scale involves patients assigning a number between 1 and 10 to . One would be “no pain,” and 10 would be the worst pain imaginable.
A non-verbal pain scale for adults may also be used to help communicate about and identify the source and severity of pain. Karen Turner, OT and Patient Navigator at Massachusetts General Hospital, explains:
Karen Turner, OT, is a Patient navigator at the Massachusetts General Hospital in Boston
The Massachusetts General Hospital Patient Accommodations Care Plan is useful communication tool that allows patients and families to document important conditions and behaviors that clinicians should know, including pain.
More information
Neuroscience News on People with Autism Experience Pain at a Higher Intensity
Recent research on autism and pain in adults.

Sibling Relationships
Communication is key to building healthy relationships and smooth transitions among family members.
Brothers and sisters, or siblings, are often key players for autistic adults and their caregivers, especially during transitional times. Research shows that autistic people who have siblings develop better social skills as well as a built-in resilience.
If an autistic person has more than one sibling, they are likely to have a different relationship with each. For example, some siblings may be able to provide strong emotional support, while others may be better at helping with, or taking on, decisions about finances and care. These roles can evolve across the lifespan, so it’s important that siblings try and maintain positive communication — not only with the autistic adult, but with one another.
Unique family dynamics
As in any family, sibling relationships change over time, but there can be unique challenges for both the autistic adult and their siblings during different stages of life. For example, older siblings might feel a sense of responsibility toward their autistic sibling and feel tentative about building a life outside the family unit. Younger siblings gain independence and develop skills and relationships that lead them to surpass their older, developmentally delayed autistic sibling. When this happens, autistic adults may struggle with feeling abandoned or jealous when a younger sibling moves out, gets married, or has children, while siblings in turn can feel guilty about becoming more independent.
Navigating sibling milestones
The goal for caregivers is to encourage the autistic adult to accept and adapt to the changes in routine and family structures, to ensure that siblings feel empowered to build independent lives while maintaining family connections. It’s productive to have conversations with the autistic adult about sibling life milestones in advance, to the extent that it’s possible. For example, when siblings prepare to leave home, caregivers can address:
how daily routines will change
when siblings will come home or when family will visit them
whether a sibling’s space or room will stay the same or be used for something else
ways siblings can communicate regularly (email, letter, video call).
Caregivers can help siblings by encouraging and supporting their life choices outside of the family home and communicating regularly about any changes in care, employment supports, and living arrangements with their autistic sibling. Keeping siblings informed about specific and general caregiver responsibilities gives them a chance to consider what role they may feel comfortable playing during their autistic sibling’s later years.
Resources for siblings
As attuned as caregivers can be to the needs of all of their children, parents who did not grow up with an autistic sibling can’t always empathize or understand the impact of autism on siblings. For most siblings, autism has punctuated their entire childhood. Siblings often benefit from talking with other siblings of autistic people or speaking with a therapist familiar with the dynamics of families touched by autism.
Because anxiety and depression are more common among siblings of autistic people, it’s important to assure that support and care are readily available. For families of people whose autism includes challenging behaviors, Autism Speaks has a guide for siblings and a Q&A that addresses some of those issues.
Sibling roles as caregivers age
Just as setting expectations and arranging for visits and regular contact is key when siblings first leave home, communication becomes increasingly important as caregivers and autistic adults get older. Family gatherings and holidays can be stressful for siblings if it is assumed they will replicate childhood rituals or vacation in the same place every year. Siblings can assist in skillfully introducing new activities alongside longtime family traditions, which serves to lighten the load on caregivers and prepare for transitions of care.
Another key consideration for siblings is how to plan for the time when parents, caregivers, or guardians can no longer provide care or support for the autistic adult. This is especially challenging when an autistic adult still lives at home. Siblings need to understand what caregivers do day-to-day long before this transition occurs, so that they are prepared to make decisions about care and support when the time comes.
Some things to consider:
How well do the siblings get along with their autistic sibling?
How do the neurotypical siblings get along with each other?
Have siblings been made aware of financial arrangements for their autistic sibling?
Are siblings prepared to advocate for the autistic adult?
Do siblings understand the medical needs of the autistic adult?
Caregivers can create opportunities to discuss and answer these questions and incorporate them into plans as they approach later transitions.
Learn more
AAHR article on Family Support and Wraparound Services
The Profound Autism Alliance has a Sibling Action Network
Autism Speaks: A Sibling’s Guide to Autism
Autism Speaks Q&A: Supporting Siblings of Autistic Children with Aggressive Behaviors
How to Bring Adult Siblings Into an Autistic Brother’s Life by Susan Senator in Psychology Today
The Sibling Support Project has resources and trainings for siblings of people with developmental disabilities
Autism Spectrum News on Adult Sibling Support
The Autism Science Foundation has a site with multiple resources for siblings, Sam’s Sibs Stick Together
Navigating Grief and Loss: A Guide for Siblings of people with IDD
Next steps: Starting the Conversation: Future Planning and Siblings of People with IDD.

Dietary Plan Tool for Schools and Day Programs
Autistic adults with special dietary needs and behaviors around food can benefit from a form that outlines those needs and the best interventions for use at school or day programs.
Autistic adults with special dietary needs and behaviors around food can benefit from a form that outlines those needs and the best interventions for use at school or day programs. Many school districts have a similar form for the school nurse but that information doesn’t always follow the adult after they turn 22.
We’ve designed an easy-to-use template based on the dietary information school districts require.

The Language of Autism
The saying goes, “if you’ve met one person with autism...you’ve met one person with autism.” The breadth of experience of autism is vast, and we want to address autism in...
The saying goes, “if you’ve met one person with autism…you’ve met one person with autism.” The breadth of experience of autism is vast, and we want to address autism in a way that respects this. For example, self-advocates often find that referring to autism as a disorder is offensive, while the families of those with autism requiring more substantial support want it to be clear that their experience of neurodiversity is quite disabling and qualifies as a disorder.
The changing language around autism
The words we use to talk about autism are continuously changing and evolving. The more linear language, including terms such as high-, moderate-, and low-functioning, has generally fallen out of favor because these terms fail to communicate that autism is characterized by splintered skills. A person with limited verbal communication skills can have intellectual acuity and great empathy, while someone who is highly verbal can be emotionally dysregulated and have extremely narrow interests that make it difficult for them to navigate the world. Very often it’s been the verbal skills that have dictated the “functioning” label, which has led to the proper conclusion that it’s an unfair and outdated measure.
Diagnostic criteria and “labels”
The current DSM-5 Criteria widened the diagnostic umbrella by removing Asperger’s Syndrome as an official diagnosis. However, while removing Hans Asperger and his ties to Nazis and eugenics was the right thing to do, that leaves people who have embraced the “Aspie” label identity adrift. The neurodiversity movement has tried to address this, and has not only shifted the lens from a purely medical model to a more social model of disability, but it has also empowered many autistic people to embrace their neurodiversity and find community with like-minded peers. Many self-advocates now proudly claim to be neurodivergent or “neurospicy.” Proponents of the autistic-led neurodiversity movement consider autism as something to be celebrated while also recognizing their support needs.
At this writing, the DSM-5 lists three levels of autism that are determined not by a person’s specific abilities but by the level of support they require:
Level 1: requires support
Level 2: requires substantial support
Level 3: requires very substantial support
These categorizations are useful for doctors and other health care professionals. For those in the support and social communities, however, such labels can seem detached and “deficit” rather than “strength” focused. It is important to remember that labels can provide a framework with which to understand each other and ourselves. It can help an autistic person and their loved ones understand why they find some things so difficult, and also why they might excel in other areas.
Our language will evolve with yours
Many patients and families have generously agreed to appear on this site and in our clinical course and we’ve consulted with them in regard to language. We share these choices with humility, recognizing the importance of evolving the understanding of autism, how that is reflected in the language we use and what it means for individuals and families.
We use both person-first language (e.g., person with autism), as well as adjective-first language (e.g., autistic person) on this site. For some members of the autism community, using adjective-first language is preferable to signify a sense of identity rather than a more medicalized “condition.” We have taken some cues from the most up-to-date language recommendations available via the American Medical Association, which also informed the choices in our clinician course.
We at AAHR will revise and adapt the language on the site as best we can to meet the needs of everyone in the autism community. We may not always get it right the first time, but we will always do our best to honor the most respectful and inclusive language. Regardless of the language that we use on this site, the intent is always to incorporate wording that is accessible, inclusive, and reflective of the priorities of the autistic community.

Planning for Medical Emergencies
Everyone—autistic people and neurotypical people—can benefit from planning for medical or mental health emergencies.
Be ready: Make a 'Go Bag'
Emergencies are easier to handle if information and supplies are at the ready. Keeping a Go Bag near the door or in the car can help.
The Go Bag – a printable list of things to have on hand to help prepare for emergencies
Start by calling the PCP
Everyone—autistic people and neurotypical people—can benefit from planning for medical or mental health emergencies. If a trip to the emergency department (ED) is necessary, you’ll want to alert your primary care provider’s office (another person in the household can make this call as necessary). It’s especially helpful to request that the PCP call ahead and let the ED or hospital know that an autistic patient is on the way and they can share any pertinent information that can be helpful for your care.
Make a call tree
Another key part of the plan is to create a call tree that includes someone in the circle of support who can contact others who should be alerted to the emergency. This information should be clearly displayed in a prominent position in your home. This is especially important for first responders-police, fire, and EMS – in case you are alone during an emergency. The call tree contacts can include service provider or group home staff, neighbors who can assist with caring for others in the family, and extended family.
Register with the local police
Most local police departmetns have a way of registering citizens with special health needs. If there are details they should know about how autism presents in you or the adult in your family take a moment to communicate about those concerns. For example, some people panic and hide when they hear sirens, see someone in uniform, or even hear the doorbell.
Calling 911
Most clinicians’ offices direct people in crisis to the local emergency department or urgent care center. If calling 911 is the best or only option, clearly state to the dispatcher that the patient is a person with autism and let them know about any communication or behavioral challenges that might be misunderstood. Many first responders are trained to interact with autistic people but many are not – it’s important to know ahead if time if local police, fire, and EMS are trained in working with the autistic community. Autism Speaks has a guide for first responders that can be shared with local public safety organizations, including information for dispatchers. In addition, there are several programs that train first responders to safely interact with autistic people, including Autism Alert and Autism Risk and Safety Management.
Tips for interacting with first responders
Whether an emergency occurs in the home or out in the community, an autism ID can be useful. It can be a simple card with details that are specific to the individual and can help avoid misunderstandings in stressful situations. Caregivers can share an ID card or self-advocates can carry them and share as necessary.
The card be shared with first responders or with staff and clinicians in emergency departments, urgent care, and hospitals. There are Medicalert IDs for autism and also sites that can create an autism ID for a fee. This one was created using a free site called Canva:
A sample identification card that outlines what strategies autstic people can use to communicate in an emergency
Mental health emergencies
When there’s a mental health emergency, think carefully about what the goal is for taking someone to the Emergency Department. Dr. Robyn Thom, a psychiatrist at the MGH Lurie Center for Autism, discusses expectations for a mental health care visit to the Emergency Department:
Dr. Robyn Thom on things to consider when going to the emergency room for a mental health emergency.
A 3×5 identification card to print and use for communicating in an emergency

Successful Telehealth Appointments
Telehealth can help those who don’t live near an autism specialist or other care provider, or if it is difficult to go to appointments in person.
Some healthcare appointments don’t require an office visit and instead can take place via telehealth. Telehealth visits usually occur using a secure videoconference platform on a personal computer, tablet, or other mobile device.
Telehealth can be useful for some types of evaluations, such as a wellness check-in or certain parts of neuropsychological exams. Each provider will have specific guidelines about when a telehealth visit may be substituted for an in-person visit, so be sure to ask.
Does insurance pay for telehealth?
The rules about telehealth coverage have changed since the end of the pandemic emergency. Check with insurance providers to see which telehealth visits are covered. It is also a good idea to see if the provider plans to offer and bill for these visits over the long term.
Benefits of telehealth
A successful telehealth appointment depends on whether the patient and provider are both comfortable with the technology and don’t mind communicating remotely if a private, quiet space is accessible. Telehealth can help those who don’t live near an autism specialist or other care provider, or if it is difficult to go to appointments in person. Some benefits to patients include:
a home or familiar environment is less stressful compared with a clinical setting
fewer transitions involved like travel, wait times, and noisy spaces
avoiding the logistics, time, and cost of travel
it can be easier to include many members of the care team (clinicians, family members, and group home/provider staff).
Downsides of telehealth
Telehealth may not be a good choice if/when
A physical examination or in-person treatment is necessary
There’s a problem that is difficult to describe or see over video (e.g., abnormal movements)
Certain tests are required, such as blood draws
The patient is not comfortable communicating via video or by phone
The patient is inclined to get distracted or wander off when not engaging in person.
Keys to a good telehealth visit
Tips for a successful telehealth appointment:
Use a private, quiet indoor space — telehealth from a car (never a moving one!) should be for emergencies only.
Make sure there’s a strong, stable internet connection on the device.
Ideally, use a device with a stable camera that can stand alone — a tablet or desktop computer is preferable to a phone.
Two or three days before the appointment, test the video software, the internet connection, camera, and microphone to make sure everything is working and that video and sound are clear.
At the start of an appointment, give the provider a contact phone number in case the connection is lost.
While a caregiver may help with communication or give information to the clinician, the autistic adult should be available to appear on camera for as much of the visit as possible.
ECHO for Autism is a good resource for providers and patients to learn more about using telehealth to deliver care.
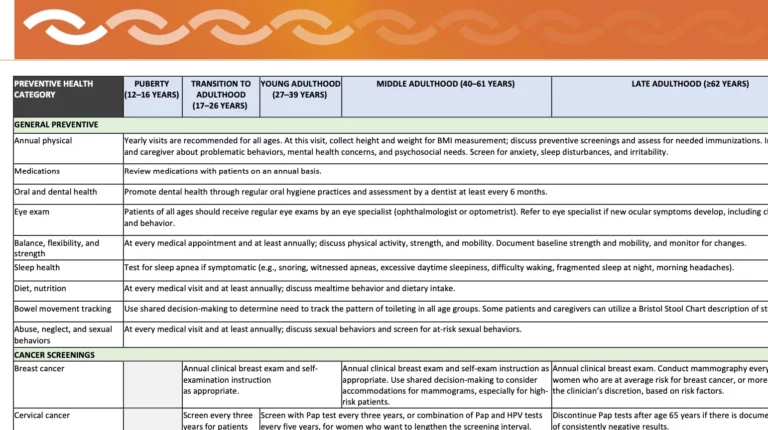
Useful Information about Preventive Care
As part of its free course, Clinical Care for Autistic Adults, Harvard Medical School developed a useful time line for preventive health care screenings and immunizations for autistic adults.
This downloadable and printable Autism Preventive Health Table was developed as part of the Harvard Medical School’s course, Clinical Care for Autistic Adults. It lists baseline preventive health care screenings and immunizations for autistic adults. The intended audience is primary care physicians but feel free to use as a reference and to share with your PCPs or other providers. Key points for caregivers and self-advocates to note:
Schedule all annual exams well in advance so that the appointment happens at a time of year and time of day that works best for the patient/family.
If possible, gather information about health conditions that can run in families such as heart problems, cancer, diabetes, depression, and addiction. This information can help identify the most important screenings and how often they should be done.
A guide to share with providers for preventive health care
The information on the table is based on the following sources:
Adult Immunization Schedule by Age, CDC, 2023.
CDC: Cancer Screening Tests. Accessed on April 1, 2023.
Dhanasekara CS, Ancona D, Cortes L, et al. Association Between Autism Spectrum Disorders and Cardiometabolic Diseases: A Systematic Review and Meta-analysis. JAMA Pediatr. 2023;177(3):248-257. doi:10.1001/jamapediatrics.2022.5629
Isenberg BM, Yule AM, McKowen JW, Nowinski LA, Forchelli GA, Wilens TE. Considerations for Treating Young People With Comorbid Autism Spectrum Disorder and Substance Use Disorder. J Am Acad Child Adolesc Psychiatry. 2019;58(12):1139-1141. doi:10.1016/j.jaac.2019.08.467
Massachusetts Department of Developmental Services Adult Screening Recommendations 2019, Mass.gov.Accessed on April 1, 2023.
Schick, Elizabeth, Is It Safe to Sedate our Son at the Dentist? Autism Speaks. 2014. Accessed on April 1, 2023.
Screening and Preventive Interventions for Oral Health in Children 5 Years and Older and Adults, U.S. Preventive Services Task Force. Accessed on April 1, 2023.
Sexually Transmitted Infections Treatment Guidelines, 2021, CDC. Accessed on April 1, 2023.
Dr. James Bath, a primary care physician for autistic adults at the MGH Lurie Center for Autism, discusses the importance of preventive care as key to a long, healthy life:
Dr. James Bath, Adult Primary Care Physician at the MGH Lurie Center for Autism

Patient Navigators
A patient navigator helps patients and clinicians create and access autism-competent care. They focus on improving processes for both inpatient and outpatient care in a medical facility and identify opportunities...
A patient navigator helps patients and clinicians create and access autism-competent care.
They focus on improving processes for both inpatient and outpatient care in a medical facility and identify opportunities to improve outreach so patients and staff are aware of the tools and resources that can improve care and outcomes. Some patient navigators specialize in assisting cancer patients but in the context of autism they work with providers to enhance their understanding of an autistic person’s unique communication, sensory, and behavioral needs.
Patient navigators also coordinate care and seek out opportunities to improve outreach in ways that heighten awareness of the specific needs that make healthcare more accessible and comfortable for autistic people.
While the work of a patient navigator is largely within the healthcare setting, they can also work with autistic adults to develop tools outside of the office environment to help with recovery from medical procedures and to assure continued good health. Such supports could include physical exercise or accommodations at home to help with mobility, guides for personal care, or communication tools for working with physical therapists.
Meet Karen Turner
Karen Turner is a patient navigator at the Massachusetts General Hospital in Boston, MA, and has developed tools and strategies for autistic people that have vastly improved the health outcomes for people with some of the most challenging forms of autism. She emphasizes the importance of creativity and flexibility in building in accommodations for autistic people and notes that she has ‘never seen an unreasonable accommodation’ for someone with autism.
Check the local hospital or clinic website to see if they list a patient navigator. While not every medical facility hospital has one it’s always wise to ask hospitals who on their staff is designated to help people with sensory needs, intellectual disabilities or communication challenges get the care they deserve. Many hospitals have clinical social workers who can be helpful in some of the same ways. Asking for accommodations is a form of advocacy and reinforces the need for these types of support staff positions to improve high quality care for autistic patients.
In this video, Karen gives advice about choosing a medical specialist.
Karen Turner, Patient Navigator at Massachusetts General Hospital, on choosing a medical specialist
Insurance

Mental Health Parity
All interaction with the insurance company, including phone calls, needs to be documented in writing. Email is okay as long as it’s clear that any information shared comes directly from the insurer.
The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) requires insurance companies to cover mental, behavioral, and substance use care equal to/in the same way as physical health care. For example, under this law, if an insurance plan pays 80% of the cost of seeing a clinician within their insurance network, then by law it wouldn’t matter if that provider was a PCP, an ear-nose-and-throat doctor, or a psychiatrist. The Mental Health & Autism Insurance Project works to explain the MHPAEA and ensure that this law is enforced.
In September, 2024, the U.S. Departments of Health and Human Services (HHS), Labor, and the Treasury released new final rules implementing MHPAEA. While the practical implications of these changes will require greater explanation before they are implemented in January of 2025 and 2026, there’s a fact sheet with some details available now.
Do all insurance plans have to follow the MHPAEA?
There are still some insurance plans that are not required to follow the mental health parity law. These include:
Medicare
U.S. Department of Defense/Tri-Care
some Medicaid plans (fee-for-service plans)
some non-federal government plans
some workplace plans that have fewer than 50 employees
plans that have been active since before March 2010.
The National Alliance on Mental Illness (NAMI) has information on mental health parity. This includes a list of benefits and services that must be covered equally. For autism, there are also state-by-state mandates.
Recognizing disparities in mental health coverage
Even though the law requires the same level of coverage for mental and behavioral health and physical health care, it’s clear from the list above that many plans aren’t required to cover mental health, while other plans have been effectively avoiding it or under-covering it. People with Medicaid coverage can use this interactive map with contact information for the Medicaid Director in each state.
ParityTrack is an organization that follows mental health parity compliance state by state. It provides information on laws passed in each state and how they affect the mental health services delivered. For example, a 2018 Iowa law requires insurance companies to cover telehealth visits.
The U.S. Department of Labor (USDOL) is responsible for ensuring that insurance companies comply with the MHPAEA. The USDOL has advice about mental, behavioral, and substance use benefits, and explains how the organization enforces the mental health parity law.
Read the news release about the Department of Labor’s 2022 report to Congress on insurance companies and mental health parity.
If care is denied, file an appeal
It takes effort to appeal an insurance claim, but if a claim is denied, appealing is one way of petitioning for coverage. When a claim is denied, the written notification will include instructions for filing an appeal and a contact number for questions.
All interaction with the insurance company, including phone calls, needs to be documented in writing. Email is okay as long as it’s clear that any information shared comes directly from the insurer.
If there’s proof an insurance company has broken the law in denying rightful mental or behavioral health care, another way to take action is to report the violation to The Kennedy Forum.
Advocate for enforcement and more for autistic people
Register to be part of the Grassroots Advocacy Network at Autism Speaks. This network works to raise awareness of the needs of people with autism and enforce laws that protect autism care.
Visit the Mental Health America Advocacy Network for a toolkit to improve compliance by contacting state legislators, and more.
For valuable information about appeals, consult the Autism Law Summit’s ABA Authorization and Appeals Playbook.

Finding Autism-Competent Health Care
Why do we call it “autism-competent health care” instead of “autism-friendly health care?” Because medical providers can be friendly but not understand the best way to treat autistic patients. It’s an education issue, not an attitude issue.
Why do we call it “autism-competent health care” instead of “autism-friendly health care?” Because medical providers can be friendly but not understand how best to care for autistic patients. It’s an education issue, not an attitude issue.
For autistic people, it can be easier to avoid seeking care because both the process and the medical environment itself are too overwhelming. This can be due to the distractions caused by sounds and lights in the clinic, verbal instructions that are too quick or unclear, touch during exams that feels uncomfortable, or procedures like blood draws that are extra painful. Making appointments, getting to the office, and navigating through the steps of an office visit can all prove difficult, too. AAHR provides help on all of these fronts and more.
Most providers who care for adults understand neurodiversity, but not all of them know best practices when it comes to treating adults with autism. Harvard Medical School has created a clinician course to bring providers important knowledge about caring for autistic adults. Yet, autistic patients need to find good care now.
Get more specifics in our article What’s an Autism-Competent Office?
Resources to Help Find Autism-Competent Care
ECHO Autism has a directory for finding clinicians trained in best practices for treating autistic children and adults.
Psychology Today has an excellent directory for finding therapists, many of whom provide autism-competent care.
The AASPIRE Toolkit is a good resource that can help patients find an adult provider who understands autism-competent care.
Got Transition? has many key resources to guide autistic young adults and their families through transitions in medical care. Their Implementation Guides are especially useful in navigating the medical transition to new providers.
Help Clinicians Learn to Provide Autism-Competent Care
While most healthcare professionals understand neurodiversity, many do not know best practices when it comes to caring for autistic adults. Harvard Medical School’s CME accredited course, Clinical Care for Autistic Adults, can fill this knowledge gap.
Share the link or the QR code for access to this training for those who care for adults. The course is free and open to anyone, including patients and caregivers.

Insurance: Turning 26
For an autistic person on a parent’s health plan, part of managing adult health care is researching and understanding the options for health insurance as age 26 approaches.
Adult health care insurance under a parent's plan usually ends at age 26
For an autistic person on a parent’s health plan, part of managing adult health care is researching and understanding the options for health insurance as age 26 approaches.
The significance of age 26
Under U.S. law, insurance plans are required to pay for the care of dependents (someone who depends on a parent’s income) up to age 26. This is true even if that person:
gets married
gives birth or adopts a child
is working, unemployed, or in school
lives in another location, not with the parent
is not listed as a dependent on the parent’s taxes
is eligible to get health insurance through their own employer.
For more information about staying on a parent’s plan until age 26, visit the Healthcare.gov site for people under 30.
Staying on a parent’s health care policy after 26
Dependents with a diagnosed disability are often able to remain on a parent’s health insurance plan past age 26. A formal medical diagnosis of autism spectrum disorder (ASD) counts toward this exception and requires proof of disability from a medical provider, such as a pediatrician, primary care provider, or psychiatrist. The insurance company will provide a form for the clinician to complete, and if there is guardianship in place, providing proof of guardianship can also help establish eligibility. The adult dependent’s permanent address should match the policy holder’s.
Key language: The medical provider should include language that the disabled dependent has “lack of substantial gainful employment” (i.e., the autistic adult cannot work full-time due to their disability), and thus cannot access employer health insurance and must remain on the parent’s health plan. The insurer usually responds with a letter approving the dependent’s status, and employers may request a copy of this document to confirm this extended coverage for their company files. The approval letter will often state that the extended coverage is valid for a specified length of time. Keep in mind that the insurer can require proof of eligibility at any time, so be sure to keep any related paperwork organized and accessible.
Key notification: Be sure to notify the insurance company as soon as possible of the plan to keep an autistic adult on a parent’s insurance after age 26. It often takes months for the insurance company to grant final approval, so discussions with the insurance company should start when:
the autistic adult turns 25, and
the open enrollment period for the parent’s insurance plan is approaching.
If the parent with the insurance changes jobs or insurance carriers, coverage for the disabled dependent usually continues; however, you may need a new approval. Check with both the current and new insurance companies to ensure continuity of care.
Getting back on a parent’s policy after 26
Once an individual is removed from a parent’s health insurance policy, it is extremely difficult to get back on. This is something to consider carefully, as it may make sense for an autistic adult to stay on a parent’s policy longer, rather than be removed and unable to rejoin if necessary.
Private insurance plus Medicare and/or Medicaid
When an adult over age 26 is on a parent’s private insurance policy and also has Medicare, the private insurance is usually primary (claims go there first) and Medicare is the secondary insurance. If the autistic adult is also on Medicaid, that insurance is the third option and is called tertiary insurance. In this instance, the clinician or hospital files insurance claims in this order:
Private insurance, then Medicare, then Medicaid
If the private insurance doesn’t cover a claim, it is sent to Medicare, then to Medicaid. Any rejected claims will arrive in the mail (these are usually marked “this is not a bill” but appear as such), but no payment should be forthcoming until an actual bill arrives from the provider confirming that the claim has been through all possible insurance processes. This can take weeks or even months.
The small employer exception
If the parent works for a small business that has 100 or fewer employees (20 employees for people over 65), then Medicare is the primary insurance for the autistic adult. In this case, claims processing will flow in the following order:
Medicare, then private insurance, then Medicaid
The claims process is handled entirely through the provider, but more often than not, processing and approval takes months rather than weeks. Again, it is best to wait until an actual bill arrives before paying the claim or filing an appeal.
Learn more about young adult insurance coverage from the U.S. Department of Health & Human Services.
Individual health care insurance from the Affordable Care Act (ACA) health insurance marketplace
Autistic adults who opt to leave their parent’s health care coverage (if they qualify) and are not employed or are opting out of their employer’s health coverage can apply for health insurance plans through the U.S. health insurance marketplace at Healthcare.gov. Just as with an employer’s insurance plan, changes to Affordable Care Act (ACA) coverage are typically offered once or twice a year during specific enrollment periods. Visit the Healthcare.gov Quick Start Guide to learn more about how to find plans and when to enroll.
Anyone qualifying as having a special health care condition (which may include autism) may be eligible to get insurance at a lower cost through Healthcare.gov. Learn more about insurance for people with special health care needs.
Healthcare.gov offers specific advice about health insurance options for young adults.
What happens when a younger disabled adult becomes eligible for Medicare? See the Insurance Resource Center for Autism and Behavioral Health’s fact sheet. (Note: the fact sheet says it’s for Massachusetts, but most of the information on it also applies to people who live outside Massachusetts.)
Finding Help With Autism Insurance Coverage
All 50 states have laws that say insurance companies must pay for autism treatment, although what is covered can vary. For those with private insurance coverage, the first step is...
All 50 states have laws that say insurance companies must pay for autism treatment, although what is covered can vary. For those with private insurance coverage, the first step is to find out what your plan is and then look up what kind of coverage for autism each state requires. The National Conference of State Legislatures provides information about autism coverage in each state. In addition:
Get more information on state regulations for health insurance plans from Autism Speaks.
Find the local Autism Society to research healthcare options.
Medicaid or Medicare?
Understand the differences between the two in our article on medicare and medicaid for autistic adults. The reason this page doesn’t include links to Medicare coverage for adults with autism is that Medicare does not, at this time, cover the same behavioral health services covered under Medicaid. The best way to get the most up-to-date information about Medicare coverage is to contact them directly at 1-800-MEDICARE.
Find the Health Insurance Marketplace website for each state
The Department of Health and Human services explains how the Affordable Care Act works regarding autism coverage.
Healthcare.gov explains health insurance options and how to qualify for Medicaid or requalify if coverage has lapsed.
Locate the nearest Developmental Disability Council
Every state has a Developmental Disability Council with useful resources on insurance and more. The National Association of Councils on Developmental Disabilities has a directory that leads to the Council in each state.
Find the local Medicaid director
People with Medicaid coverage can use this interactive map with contact information for the Medicaid Director in each state.
Check the U.S. Department of Health & Human Services
The U.S. Department of Health & Human Services Interagency Autism Coordinating Committee (IACC) offers a range of helpful information on state resources for autism, insurance, and health coverage. Some are for children, but many apply to autistic adults, too.
For national and state-specific information see the IACC’s Agencies and Organizations page.
For Massachusetts families – and beyond
The Insurance Resource Center for Autism and Behavioral Health, part of the E.K. Shriver Center at UMass Chan Medical School, has helpful information and resources on their website, www.massairc.org. They primarily assist Massachusetts residents, but much of their information is also helpful for those who live outside of the state.
Advocate for better coverage!
It’s also a great idea to advocate for better coverage from private insurance, Medicare or mental health parity. Help improve the system – start by contacting legislators through the National Conference of State Legislatures.

Medicare for Older Adults and Caregivers
For caregivers whose autistic adults already have Medicare or Medicaid, any change in insurance must be reported to Medicare as soon as possible — even if it is simply changing from one employer’s insurance to another. Medicare requires current information for all guardians of adults on Medicare or Medicaid.
Medicare age requirements
Medicare is the U.S. government health care program for adults ages 65 and older. It is also available to adults ages 18 to 64 who have certain disabilities.
There are many special circumstances that can affect Medicare enrollment. Regardless of the age when applying, everyone should consult the Medicare guide for beginning coverage.
The two most common times to enroll in Medicare are:
at age 65 (when many people retire). The enrollment period starts three months before the 65thbirthday, and ends three months after that.
after age 65, when employer insurance coverage ends. The current deadline is eight months after coverage ends, so it’s important to apply before that window closes.
Autistic people who did not qualify earlier in life (as well as their caregivers) are eligible for Medicare once they turn 65. Learn how Social Security benefits are linked to Medicare.
What happens when a younger disabled adult becomes eligible for Medicare? See the Insurance Resource Center for Autism and Behavioral Health’s fact sheet (the sheet says Massachusetts, but most of the information applies to people who live outside of Massachusetts).
Important: For caregivers whose autistic adults already have Medicare or Medicaid, any change in insurance must be reported to Medicare as soon as possible — even if it is simply changing from one employer’s insurance to another. Medicare requires current information for all guardians of adults on Medicare or Medicaid.
Find the date you can sign up for Medicare. Learn the basics of Medicare.
What does Medicare pay for?
Medicare covers specific health care expenses. The parts of Medicare include:
Medicare Part A – Everyone who signs up for Medicare receives Part A, which covers hospital care, nursing care, and hospice.
Medicare Part B – Everyone who signs up for Medicare also receives Part B, which covers medical expenses such as seeing a clinician or other health care provider.
Medicare Part C – Additional insurance to cover what Medicare Part A and Medicare Part B do not cover. You can choose a Medicare Advantage plan from a private insurance company. It is still Medicare, but a private insurance company oversees it.
Medicare Part D – Optional insurance to help pay the cost of prescription drugs. Medicare Advantage plans usually include a drug coverage plan.
The Medicare site has a page that explains how it works with private insurance and who pays for what.
Signing up for Medicare
Visit www.Medicare.gov or this sign-up page.
Still have questions and want to talk to a person? Call 800-MEDICARE (800-633-4227).
Gender-Specific Care

Menstruation & Premenstrual Syndrome (PMS)
There is more openness around discussing female reproductive health than when many current adults entered puberty, and more and better options for managing menstruation and PMS.
Autism is not known to affect when menarche (the onset of menstruation) occurs, which is usually between the ages of 11 and 13. Many factors can affect when a first period occurs, including but not limited to:
overall health
family size and health history
health and nutrition habits
psychological factors, such as stress
environmental factors, such as exposure to toxins
socioeconomic and demographic status.
Hygiene and routine care
Establishing routines for good hygiene is key to maintaining positive health through the lifespan of autistic women. There is more openness around discussing menstruation as well as options for managing related issues, compared to when many current adults started puberty. A PCP, family practitioner, or gynecologist can advise patients and caregivers about information and issues surrounding menstruation. Clinicians and caregivers can consider where autistic patients are in their reproductive timeline to ensure an understanding of topics such as:
terminology and language for talking about menstruation
blood flow and frequency, and what characterizes a “normal” period
importance of menstrual calendar and cycle tracking
how to manage tampons, cups, pads, and period-proof underwear
role of caregivers or group home staff in monitoring and assisting menstrual processes to assure good hygiene.
Side effects and symptoms
Menstruation is not static; physical and emotional changes continue throughout a woman’s reproductive years. What is normal for one person may not for another. Recent studies indicate that autistic women have higher rates of menstrual issues than is typical of their peers, such as irregular cycles, painful periods (dysmenorrhea), and excessive bleeding. Cramps, nausea, and abdominal pain are common side effects; however, any changes in intensity or frequency should be discussed with a woman’s clinician, especially if they are severe enough to interfere with the ability to work or attend school.
Premenstrual syndrome (PMS)
Physical and behavioral symptoms related to cyclical hormonal fluctuations that occur before a period begins are known as premenstrual syndrome (PMS). PMS is more common in autistic women and can be particularly difficult to manage. Symptoms such as the ones listed below should be brought to the attention of a woman’s clinician:
Physical
changes in appetite
fatigue
migraines
nausea
seizures
worsening irritable bowel syndrome
Emotional
anxiety
depression
mood swings
aggression toward caregivers.
Addressing menstruation-related Issues
In some cases, patients and caregivers may want to consider menstrual suppression to provide relief for menstruation-related mood and behavior changes. Contraceptive medications are typically used to suppress the hormones that control menstrual flow. The decision to use these medications should be discussed among the patient, clinician, and, where appropriate, the caregiver/guardian who helps with medical decision making. That conversation should include discussing:
interactions between contraceptive medication and other medications
medical or digestive issues, such as IBS, that might affect the absorption of contraceptive medication
risk factors for potentially dangerous side effects, such as blood clots
the rationale for using contraceptive medication and its impact on decisions surrounding sexual activity
risks and privacy considerations for patients who live in independent and group home settings
revisiting contraceptive medication decisions as women approach midlife and menopause.
Learn more:
The Autism-Friendly Guide to Periods by Robyn Steward
The National Library of Medicine fact sheet on Menstrual Suppression
From Harvard Health:
Heavy Menstrual Periods
Endometriosis
Gyn Care 101: What to know about seeing a gynecologist

How is Autism Different in Women?
Autism is a diverse condition that affects individuals of all genders. Although it is still more commonly diagnosed in males, recent research suggests that the disparity is shrinking as awareness of how autism presents in females increases.
This article is based on a LurieNOW article by Dr. Alyssa Milot Travers, a licensed psychologist at the Lurie Center for Autism with specific expertise in women on the autism spectrum. Dr. Travers is also an Instructor in Psychiatry at Harvard Medical School.
Autism is a diverse condition that affects individuals of all genders; the overall prevalence estimate of autism in the U.S. is one in 36 children. According to the Centers for Disease Control and Prevention (CDC), as of March 2023 about 4% of boys and 1% of girls age 8 years have autism.
Although an autism diagnosis occurs more often in men than in women, recent research suggests that autism in women may be both underdiagnosed and misdiagnosed. Recognizing and understanding how autism presents in women is crucial for accurate diagnosis, appropriate support, and targeted interventions. The evolving understanding of gender differences in autism is dismantling the notion that autism is more or less a “male condition.”
Gender identity in autism research
The majority of autism research in recent decades has focused on cisgender individuals, or those who have a gender identity that matches their sex assigned at birth. The most current research reveals that gender diversity is more common in autistic people than in their neurotypical peers. Consequently, there is a slow but distinct shift toward including gender diversity in autism research, which will provide a more accurate representation of all autistic individuals. The current knowledge of the female subtype of ASD is based on research of cisgender women.
Outward signs: Special interests and repetitive behaviors
Restricted interests and repetitive behaviors occur in autistic men and women; however, the nature of these behaviors can differ. Traditionally, clinicians have been trained to recognize stereotypical male-associated restricted interests, such as transportation, dinosaurs, or space. In contrast, autistic women may develop interests that are more closely aligned with societal norms, such as animals, art, celebrities, or literature.
This divergence can contribute to the misconception that women with these types of restricted interests are simply displaying enthusiastic hobbies rather than autistic traits. Repetitive patterns of behavior in women may manifest as classic autistic behaviors like rocking or hand/finger movements. However, they may also appear as behaviors not necessarily associated with autism, such as perfectionistic tendencies or restrictive patterns of eating/eating disorders.
Impediments to an ASD diagnosis: Overshadowing, masking, and camouflaging
Based on behavioral history, women may be more apt to receive diagnoses such as anxiety, mood disorders, learning disorders, and/or eating disorders rather than autism. This phenomenon is called diagnostic overshadowing, which occurs when a person’s symptoms are attributed to a psychiatric problem versus an underlying medical condition or a developmental delay such as autism. This can complicate the diagnostic process, as the focus may be on managing these secondary conditions rather than recognizing the underlying autistic traits.
Autistic women are also more likely to develop compensatory strategies to mask their challenges. For example, women often have stronger social imitation skills and the ability to mimic social behavior compared to men. Due to their social foundation, girls may develop one or two close friendships, helping them absorb social rules and norms. Their strong social interest may lead them to “camouflage” or compensate for social understanding and communication challenges, making these vulnerabilities difficult to detect in everyday interactions or larger classroom or employment settings. As a result of these differences, women are often more likely to be diagnosed later in life, if at all.
The Autistic Women and Nonbinary Network provides useful information and resources for gender-diverse autistic individuals.
For diagnostic resources, see our article about seeking an ASD diagnosis as an adult.
Recommended Reading and Viewing
For women:
Camouflage: The Hidden Lives of Autistic Women by Dr. Sarah Bargiela
22 Things a Woman with Asperger’s Syndrome Wants Her Partner to Know by Rudy Simone
The Autistic Brain: Exploring the Strengths of a Different Kind of Mind by Temple Grandin
Odd Girl Out: An Autistic Woman in a Neurotypical World by Laura James
From the American Autism Association: 5 TedX Talks from Women with Autism
For caregivers:
A Guide to Mental Health Issues in Girls and Young Women on the Autism Spectrum: Diagnosis, Intervention and Family Support by Dr. Judy Eaton
Girls Growing Up on the Autism Spectrum: What Parents and Professionals Should Know About the Pre-Teen and Teenage Years by Shana Nichols with Gina Marie Moravcik and Samara Pulver Tetenbaum
For partners of autistic adults:
The Other Half of Asperger Syndrome: A Guide to Living in an Intimate Relationship with a Partner Who is on the Autism Spectrum by Maxine Aston
Care Transitions

Finding Autism-Competent Health Care
Why do we call it “autism-competent health care” instead of “autism-friendly health care?” Because medical providers can be friendly but not understand the best way to treat autistic patients. It’s an education issue, not an attitude issue.
Why do we call it “autism-competent health care” instead of “autism-friendly health care?” Because medical providers can be friendly but not understand how best to care for autistic patients. It’s an education issue, not an attitude issue.
For autistic people, it can be easier to avoid seeking care because both the process and the medical environment itself are too overwhelming. This can be due to the distractions caused by sounds and lights in the clinic, verbal instructions that are too quick or unclear, touch during exams that feels uncomfortable, or procedures like blood draws that are extra painful. Making appointments, getting to the office, and navigating through the steps of an office visit can all prove difficult, too. AAHR provides help on all of these fronts and more.
Most providers who care for adults understand neurodiversity, but not all of them know best practices when it comes to treating adults with autism. Harvard Medical School has created a clinician course to bring providers important knowledge about caring for autistic adults. Yet, autistic patients need to find good care now.
Get more specifics in our article What’s an Autism-Competent Office?
Resources to Help Find Autism-Competent Care
ECHO Autism has a directory for finding clinicians trained in best practices for treating autistic children and adults.
Psychology Today has an excellent directory for finding therapists, many of whom provide autism-competent care.
The AASPIRE Toolkit is a good resource that can help patients find an adult provider who understands autism-competent care.
Got Transition? has many key resources to guide autistic young adults and their families through transitions in medical care. Their Implementation Guides are especially useful in navigating the medical transition to new providers.
Help Clinicians Learn to Provide Autism-Competent Care
While most healthcare professionals understand neurodiversity, many do not know best practices when it comes to caring for autistic adults. Harvard Medical School’s CME accredited course, Clinical Care for Autistic Adults, can fill this knowledge gap.
Share the link or the QR code for access to this training for those who care for adults. The course is free and open to anyone, including patients and caregivers.
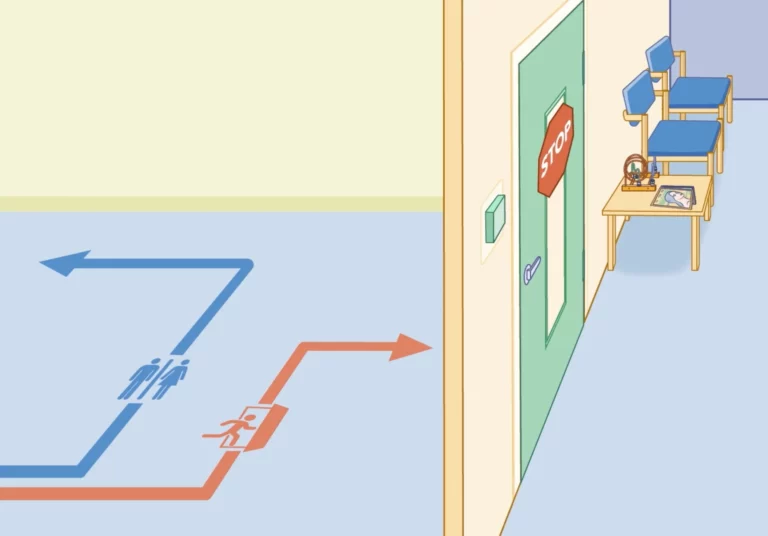
What’s an Autism-Competent Office?
Environments with tight spaces, and lots of noise and/or people are challenging for all patients, but especially those with the sensory issues that come with being autistic.
Environments with tight spaces, and lots of noise and/or people are challenging for all patients, but especially those with the sensory issues that come with being autistic.
Some of the physical characteristics of an autism-competent clinical office or hospital include:
Fewer bright lights
A neat, orderly appearance, without too many magazines, video screens, or decorations
Quiet music and overhead sounds or none at all
Fewer smells from cleaning products or disinfectants
Calm neutral colors, keeping any areas of bright color to a minimum
Easy access to electrical outlets for keeping devices charged
Socially distanced seating
A quiet room or space separate from the waiting area
An autism-competent office or hospital offers more than one way to communicate between patients and staff. These may include:
Email
Online scheduling and access to medical records (also known as patient portals)
Texting
Phone calls and voicemail
A tablet or communication board for use during an appointment
Our Clinician Course, Clinical Care for Autistic Adults, gives healthcare providers advice on how to create autism-competent spaces and train clinical staff to better serve the needs of autistic patients. The downloadable tip sheet can help patients to advocate for autism-competent care while directing clinicians on how to best provide that care.
An innovative example of autism-competent, neurodiverse healthcare can be found at All Brains Belong, a medical practice that takes a “whole life” approach.
Animation: What’s an autism-competent medical office look like?

Sibling Relationships
Communication is key to building healthy relationships and smooth transitions among family members.
Brothers and sisters, or siblings, are often key players for autistic adults and their caregivers, especially during transitional times. Research shows that autistic people who have siblings develop better social skills as well as a built-in resilience.
If an autistic person has more than one sibling, they are likely to have a different relationship with each. For example, some siblings may be able to provide strong emotional support, while others may be better at helping with, or taking on, decisions about finances and care. These roles can evolve across the lifespan, so it’s important that siblings try and maintain positive communication — not only with the autistic adult, but with one another.
Unique family dynamics
As in any family, sibling relationships change over time, but there can be unique challenges for both the autistic adult and their siblings during different stages of life. For example, older siblings might feel a sense of responsibility toward their autistic sibling and feel tentative about building a life outside the family unit. Younger siblings gain independence and develop skills and relationships that lead them to surpass their older, developmentally delayed autistic sibling. When this happens, autistic adults may struggle with feeling abandoned or jealous when a younger sibling moves out, gets married, or has children, while siblings in turn can feel guilty about becoming more independent.
Navigating sibling milestones
The goal for caregivers is to encourage the autistic adult to accept and adapt to the changes in routine and family structures, to ensure that siblings feel empowered to build independent lives while maintaining family connections. It’s productive to have conversations with the autistic adult about sibling life milestones in advance, to the extent that it’s possible. For example, when siblings prepare to leave home, caregivers can address:
how daily routines will change
when siblings will come home or when family will visit them
whether a sibling’s space or room will stay the same or be used for something else
ways siblings can communicate regularly (email, letter, video call).
Caregivers can help siblings by encouraging and supporting their life choices outside of the family home and communicating regularly about any changes in care, employment supports, and living arrangements with their autistic sibling. Keeping siblings informed about specific and general caregiver responsibilities gives them a chance to consider what role they may feel comfortable playing during their autistic sibling’s later years.
Resources for siblings
As attuned as caregivers can be to the needs of all of their children, parents who did not grow up with an autistic sibling can’t always empathize or understand the impact of autism on siblings. For most siblings, autism has punctuated their entire childhood. Siblings often benefit from talking with other siblings of autistic people or speaking with a therapist familiar with the dynamics of families touched by autism.
Because anxiety and depression are more common among siblings of autistic people, it’s important to assure that support and care are readily available. For families of people whose autism includes challenging behaviors, Autism Speaks has a guide for siblings and a Q&A that addresses some of those issues.
Sibling roles as caregivers age
Just as setting expectations and arranging for visits and regular contact is key when siblings first leave home, communication becomes increasingly important as caregivers and autistic adults get older. Family gatherings and holidays can be stressful for siblings if it is assumed they will replicate childhood rituals or vacation in the same place every year. Siblings can assist in skillfully introducing new activities alongside longtime family traditions, which serves to lighten the load on caregivers and prepare for transitions of care.
Another key consideration for siblings is how to plan for the time when parents, caregivers, or guardians can no longer provide care or support for the autistic adult. This is especially challenging when an autistic adult still lives at home. Siblings need to understand what caregivers do day-to-day long before this transition occurs, so that they are prepared to make decisions about care and support when the time comes.
Some things to consider:
How well do the siblings get along with their autistic sibling?
How do the neurotypical siblings get along with each other?
Have siblings been made aware of financial arrangements for their autistic sibling?
Are siblings prepared to advocate for the autistic adult?
Do siblings understand the medical needs of the autistic adult?
Caregivers can create opportunities to discuss and answer these questions and incorporate them into plans as they approach later transitions.
Learn more
AAHR article on Family Support and Wraparound Services
The Profound Autism Alliance has a Sibling Action Network
Autism Speaks: A Sibling’s Guide to Autism
Autism Speaks Q&A: Supporting Siblings of Autistic Children with Aggressive Behaviors
How to Bring Adult Siblings Into an Autistic Brother’s Life by Susan Senator in Psychology Today
The Sibling Support Project has resources and trainings for siblings of people with developmental disabilities
Autism Spectrum News on Adult Sibling Support
The Autism Science Foundation has a site with multiple resources for siblings, Sam’s Sibs Stick Together
Navigating Grief and Loss: A Guide for Siblings of people with IDD
Next steps: Starting the Conversation: Future Planning and Siblings of People with IDD.
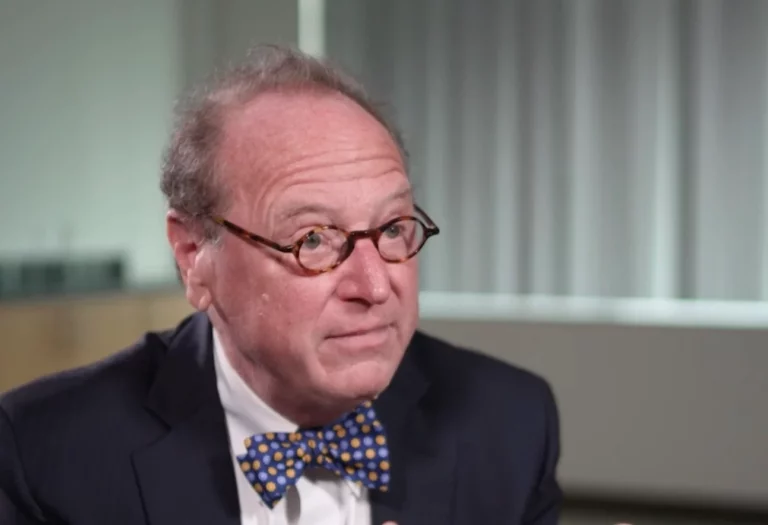
Getting an Autism Diagnosis as an Adult
The increased awareness of autism and associated neurodivergent traits in adults has led many to seek testing and/or a diagnosis.
Autism is commonly associated with childhood, the assumption being that if a person is autistic they will have received that diagnosis when they were young. This is not always the case. Some adults struggle with the symptoms and challenges associated with autism but have never received a formal diagnosis.
The increased awareness of autism and associated neurodivergent traits in adults has led many to seek testing and/or a diagnosis. Adults often consider autism when a person in their family is diagnosed and they recognize autistic traits in themselves. Because autism was long assumed to be more common in boys and men, it has traditionally been underdiagnosed in girls and women, who may still find getting a diagnosis as an adult particularly challenging.
Who can diagnose autism in adults?
Adults seeking a formal diagnosis can consult with their primary care provider, a psychiatrist, a psychologist, or a social worker to understand how best to seek an evaluation. A psychiatrist (MD), psychologist (PhD), or neuropsychologist (PhD) usually makes the medical diagnosis of autism spectrum disorder (a full neuropsychological evaluation is not required). A medical diagnosis is necessary, however, to apply for any disability benefits on the basis of an autism diagnosis.
In this video, Dr. Chris McDougle, Director of the Lurie Center for Autism, discusses the process of seeking an autism diagnosis as an adult.
Dr. Chris McDougle, Director of the MGH Lurie Center for Autism
Where to learn more about an adult diagnosis
The Association for Autism and Neurodiversity (AANE) has advice for adults seeking a diagnosis. They offer information on why a person might (or might not) want to seek a diagnosis, and what an ASD diagnosis as an adult means across the lifespan. The website also provides useful advice on finding resources for help and how to talk about being autistic with family, friends, and employers. AANE also has many online groups that provide support and a sense of community for neurodivergent adults, as well as for their caregivers and families, regardless of whether they have a formal autism diagnosis.
More resources
Autism Speaks Adult Diagnosis Tool Kit This resource explains the diagnostic process, has links to clinicians who can diagnose ASD, and provides other information useful to those considering pursuing a formal ASD diagnosis.
Formal Diagnostic Criteria for Autism The medical criteria that clinicians use to diagnose autism.
Making Sense of the Past as a Late-Diagnosed Autistic Adult by Katie Rose Guest Pryal in Psychology Today
After all these years I finally understand that there’s a scientific reason for the way I am different, and that I didn’t do anything wrong by being this way.
—Maggie C., autistic adult
Transitioning from Pediatric to Adult Care
Transitioning from pediatric to adult care can be challenging as autistic patients outgrow the services of pediatric practices and enter a fragmented healthcare system that is less familiar.
It can be a challenging time as autistic patients leave the services of pediatric practices and enter a health care system for adults that is less familiar with their needs and less prepared to meet them. There’s no required age for this transition to happen, but it is usually between the ages of 18 and 22, and can happen as late as age 26. See our articles on insurance for more information about important decisions at ages 22 and 26.
Got Transition, a site focusing on health care transitions, is a valuable resource for families and self-advocates. It offers a readiness assessment tool, a transition timeline, and a robust frequently asked questions section.
There are a few key steps involved when transitioning from a pediatrician to an adult primary care provider (PCP).
Consider a “meet and greet” pre-appointment
For autistic people who require high levels of support, setting up an additional appointment when booking the patient’s first visit with their new PCP can be helpful. It can be reassuring for caregivers to meet alone with the PCP before the patient’s first visit to establish if the clinician is indeed a good fit. (Most insurance providers will cover this kind of consultation, but it’s always good to check.) Because the transition from pediatric to adult care often comes at a time when other big transitions are afoot, it may also be helpful to talk about any planned transitions from school to work or adult services either at the caregiver-clinician visit or at the first appointment.
As part of the HMS Clinician Course, Dr. James Bath, Primary Care Provider for Autistic Adults at the Lurie Center for Autism, helped to develop an Initial Visit Patient Profile form to facilitate a positive clinician-patient exchange of the key information during this transition.
Information to bring to a primary care visit
Transfer medical records
Once the new PCP is in place, it’s important to make sure that health care records are transferred to the new practice. Be sure to include specialist records as well as those from the pediatrician. These records should include all appointment notes as well as results of lab work, imaging, or other tests, so the new PCP has access to health history as well as current medical concerns.
Tips on transferring records:
Most clinicians use electronic health record (EHR) systems to store medical data, but sometimes different vendor systems are incompatible. It’s best to ask the receiving clinician’s office if there is anything you need to do on your end to facilitate a successful handoff.
Be sure to include records from specialists and evaluations such as neuropsychological reports (if these were completed through a school district, they will not be in the electronic medical record, but digital copies should be available from the provider).
If you’ve used a patient portal, download and keep copies of all records, as you will no longer have online access to this information once you leave a practice.
The difference between Electronic Medical Records (EMR) and Electronic Health Records (EHR)
Although the terms Electronic Medical Records (EMR) and Electronic Health Records (EHR) and are often used interchangeably, there are importance differences between them. EMRs are digital patient records and charts, while EHRs are that and more. EHRs are more comprehensive and include tools for prescribing medications electronically, ordering labs, streamlining internal and external communications, and sharing data.
Medication
Some things to keep in mind about medication:
Keep a list of all medication, dosage, instructions, and prescriber information and bring it to the first appointment. Keeping a master list will help to ensure that there are no missed doses during the transition process.
Discuss both current and past medication use with the PCP, including reasons for any past medication discontinuation, so a full medication history is clear.
Remember to pass along any new medication orders to care team members who distribute medication, such as day program providers, group home staff, teachers, therapists, or home care aides.
Dr. James Bath gives advice the transition from pediatric to adult care
Care team communication
Dr. Bath reinforces the value of communication during the transition from pediatric to adult care, and establishing a role as an essential part of the health care team. He notes that “The most integral part of having a successful health care transition is that we as the providers are listening to the families and the patients, and what their experiences have been and what has been successful and what has not been so successful, because that history is invaluable.”
During the first appointment, patients and caregivers should explain how they choose to be addressed, including preferred pronouns. Many people choose to be called by their first name or a nickname, while others opt for Mr., Miss, or Ms. The use of “Mom” and “Dad” might best be left behind in the pediatric office, and generalized terms may feel uncomfortable or condescending (for example, “pal” or “sweetie”). Personal identity and the terminology around it can be especially important for autistic self-advocates, so this is a key conversation.
Susan Senator, and AAHR subject expert and parents of an autistic adult, discusses the language of autism in Psychology Today, “Please don’t call my autistic son “Buddy.”
Like a general pediatrician, PCPs coordinate care across specialties, so it’s important to make sure they are aware of other clinicians providing care. That may or may not be clear through the medical record alone, so it can be helpful to have a list of names and contact information for all specialists and other providers on hand for the PCP.
Maura Sullivan, the parent of two autistic young men, understands the need for balance when communicating about health — that everyone needs to be part of the conversation and to participate in care in whatever way they are able.
As my kids transition, I want more of their voice to be heard and less of my voice to be heard
– Maura S.
Legal Matters

The Formal Diagnostic Criteria for Autism
When a clinician makes a formal diagnosis of Autism Spectrum Disorder, they use the criteria laid out in the Statistical Manual of Mental Disorders, Volume V, 2013. It reads as...
When a clinician makes a formal diagnosis of Autism Spectrum Disorder, they use the criteria laid out in the Statistical Manual of Mental Disorders, Volume V, 2013.
It reads as follows:
Autism Spectrum Disorder
Diagnostic Criteria 299.00 (F84.0)
Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive; see text):
Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions.
Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication.
Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts; to difficulties in sharing imaginative play or making friends; to absence of interest in peers.
Specify current severity: Severity is based on social communication impairments and restricted, repetitive patterns of behavior (see Table below).
Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text):
Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases).
Insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat same food every day).
Highly restricted, fixated interests that are abnormal in intensity or focus (e.g., strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interests).
Hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement).
Specify current severity: Severity is based on social communication impairments and restricted, repetitive patterns of behavior (see Table below).
Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learned strategies in later life).
Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
These disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and autism spectrum disorder frequently co-occur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level.
Note: Individuals with a well-established DSM-IV diagnosis of autistic disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified should be given the diagnosis of autism spectrum disorder. Individuals who have marked deficits in social communication, but whose symptoms do not otherwise meet criteria for autism spectrum disorder, should be evaluated for social (pragmatic) communication disorder.
Specify if: With or without accompanying intellectual impairment
With or without accompanying language impairment
Associated with a known medical or genetic condition or environmental factor (Coding note: Use additional code[s] to identify the associated medical or genetic condition.)
Associated with another neurodevelopmental, mental, or behavioral disorder (Coding note: Use additional code[s] to identify the associated neurodevelopmental, mental, or behavioral disorder[s].)
With catatonia (refer to the criteria for catatonia associated with another mental disorder, pp. 119-120, for definition) (Coding note: Use additional code 293.89 [F06.1] catatonia associated with autism spectrum disorder to indicate the presence of co-morbid catatonia.)
Social (Pragmatic) Communication Disorder
Diagnostic Criteria 315.39 (F80-.89)
Persistent difficulties in the social use of verbal and nonverbal communication as manifested by all of the following:
Deficits in using communication for social purposes, such as greeting and sharing information, in a manger that is appropriate for the social context.
Impairment of the ability to change communication to match context or the needs of the listener, such as speaking differently in a classroom than on a playground, talking differently to a child than to an adult, and avoiding use of overly formal language.
Difficulties following rules for conversation and storytelling, such as taking turns in conversation, rephrasing when misunderstood, and knowing how to use verbal and nonverbal signals to regulate interaction.
Difficulties understanding what is not explicitly stated (e.g., making inferences) and nonliteral or ambiguous meanings of language (e.g., idioms, humor, metaphors, multiple meanings that depend on the context for interpretation).
The deficits result in functional limitations in effective communication, social participation, social relationships, academic achievement, or occupational performance, individually or in combination.
The onset of the symptoms is in the early developmental period (but deficits may not become fully manifest until social communication demands exceed limited capacities).
The symptoms are not attributable to another medical or neurological condition or to low abilities in the domains of word structure and grammar, and not better explained by autism spectrum disorder, intellectual disability (intellectual developmental disorder), global development delay, or another mental disorder.
Reprinted with permission from American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Copyright © 2013. American Psychiatric Association. All Rights Reserved. Permission from the APA is required to reproduce DSM-5 Criteria and any Related Tables.
More information from AAHR
Getting an Autism Diagnosis as an Adult
The Language of Autism
How is Autism Different in Women?

Health Care Rights for Autistic Patients
Patients, caregivers, and guardians have the right to ask questions and to get clear, useful answers. It can be especially challenging to do so on the spot or in stressful situations.
The Americans with Disabilities Act (ADA) law ensures that people with disabilities get the accommodations they need to do things such as go to school, find and keep a job, use transportation, access public spaces, and receive proper healthcare. All health care providers are legally obligated to follow this law. The more autistic people know about their rights under the ADA, the clearer they can be with health care providers about how to meet their needs.
Accommodations at a medical office or hospital
Patients and families have a right to ask their health care provider’s office, clinic, or hospital to make changes if they’re unable to receive equal access to health care. Massachusetts General Hospital’s ASPIRE program has a Healthcare Toolkit with detailed information about what the ADA requires for patients with autism and how to ask for accommodations.
Accommodations for people with autism might include:
Maps of the clinic or hospital
Options for telehealth appointments
Communication tools such as picture boards, or a tablet or phone app that explains office or medical procedures
Permission to bring a service animal into spaces where animals aren’t usually allowed
For more information, consult our article on what an autism-competent office looks like.
Do health care rights change in the transition to adulthood?
The right to good care isn’t age specific, but support services and insurance coverage often change at key age transitions. When an autistic person who receives services from the state and education system turns 22, many support services change (or go away entirely). In addition, the rights to some types of accommodations may change as well depending on how autism presents, co-existing health conditions, state of residence, and other factors.
Got Transition? has many key resources to guide autistic young adults and their families through transitions in medical care. Their Implementation Guides are especially useful in navigating the medical transition to new providers.
For self-advocates, Autistic Self Advocacy Network has a guide called the Roadmap to Transition: A Handbook for Autistic Youth Transitioning to Adulthood that offers advice on many transition-related topics, including health care. Specific chapters that might be helpful include:
Chapter 3, Know Your Rights. Rights and services autistic people have under the law.
Chapter 10, Health Care. Health care rights, how to work with a medical provider and more.
Communication tips
Patients, caregivers, and guardians have the right to ask questions and to get clear, useful answers. It can be especially challenging to do so on the spot or in stressful situations. Whenever possible, try to do the following things:
Write down questions for your health care provider ahead of time or make a checklist of points to cover.
Remember that asking for answers in writing is also acceptable.
Some providers have a patient portal that allows patients to communicate with providers privately via email. This can be used to submit questions or concerns ahead of an appointment.
Also, be prepared to ask more than once if the answers are not clear or useful the first time. Knowing that accessible healthcare is well within your rights and covered under the law can make it easier to ask for what is needed.
If it’s the first time visiting a new doctor, fill out the AAHR Initial Visit Patient Profile and bring it to the appointment.
Information to bring to a primary care visit

Guardianship for Autistic Adults
Some people with autism make their own health care and medical decisions. Others cannot or prefer to have someone help them with these decisions. When health care matters are complex...
Some people with autism make their own health care and medical decisions. Others cannot or prefer to have someone help them with these decisions. When health care matters are complex or overwhelming it might be necessary to appoint a guardian. A health care guardian has the legal right to make health care decisions for another person, with full permission to access records and communicate with providers. A health care guardian may also be called a medical guardian.
Who should consider a health care guardian?
Caregivers for people with autism who interact with their clinicians are often required to become guardians so that they can do things like make appointments, access medical records and make important decisions in an emergency. A family with an autistic person should consider guardianship if there’s difficulty with at least one area of life:
Health care: The person cannot understand, communicate and decide about their own health care.
Food and shelter: The person cannot manage money, provide their own food or place to live.
Potential for exploitation, serious injury or illness: The person cannot consistently make decisions that help them stay safe.
Whenever possible, guardians are obligated to give their autistic family member a chance to understand and weigh in on all decisions.
Lisa Nowinsky, PhD, title, discusses guardianship and medical decision making for autistic adults:
Lisa Nowinski, PhD, Director of Non-Clinician Service, MGH Lurie Center for Autism
Health care guardians and other options for autistic adults
There are several options to consider when it comes to seeking guidance for medical decision-making. They may:
Request permission for someone to see their medical information and help with decisions.
Patients must give written permission for a family member to see their health information or help with decisions. Doctors have medical release forms in their offices or on their patient portals.
Use a tool called Supported Decision Making.Supported Decision Making is a way of seeking help with complex medical decisions. The final decision lies with the patient, but they can bring other people (family, friends, support professionals, or other clinicians on their care team) into the conversation so that they make an informed choice.
Self-advocates who do not need a guardian can learn more about the kinds of support they can get from the American Civil Liberties Union’s FAQs on Supported Decision-Making.
Full guardianship.Guardianship is a legal process that often requires a lawyer, and each state has its own rules and may even have different types of guardians – it’s important to review the criteria for the state in which the autistic person lives. Legal forms are available at state government websites.
An attorney at Autism Spectrum News provides more details: Legal Guardianship: The Pros and Cons for Your Adult Disabled Child
Once guardianship is established, there are requirements for keeping it in place, usually an annual report filed in probate court (no lawyer required for that). Guardians should have proof of guardianship with them at all medical appointments and anywhere medical decisions are made. It’s a good idea to keep a copy of proof of guardianship (usually the court document awarding guardianship) in the car, backpack or purse.
Up for discussion
Guardianship decisions and the rules governing them are under review in many states as autistic self-advocates raise concerns about their right to make their own decisions. The National Council on Disability’s report Turning Rights into Reality: How Guardianship and Alternatives Impact the Autonomy of People with Intellectual and Developmental Disabilities provides useful information about the changing attitudes and legislative initiatives affecting guardianship.

Everyone Needs a Healthcare Proxy
Each member of the family should have a health care proxy that allows someone to make medical decisions if they fall ill.
Everyone needs a health care proxy, including guardians themselves. Each member of the family should have a health care proxy that allows someone to make medical decisions if they fall ill. Sometimes called a durable medical power of attorney or an advanced directive, the proxy designates a person who can determine what the patient would have wanted if they were able to talk with their clinicians about their care.
Health care proxies aren’t for day-to-day medical decisions. They only cover those times when the patient is physically or cognitively unable to make medical care decisions. For example, hospitals often require evidence of a proxy when a person has surgery under anesthesia. In this case, the proxy is only in effect for the time the person is unconscious. Once they wake up and can communicate, they regain the ability to make their health care decisions.
Lisa Nowinski, PhD, of the MGH Lurie Center for Autism, explains some of the key issues around medical decision making:
Lisa Nowinski PhD, Director of Non-Clinical Care, MGH Lurie Center for Autism
Every state is different
Proxy forms vary from state to state but often include:
Medical treatment preferences for palliative care or life-support measures that involves breathing and feeding devices.
Designating a second person as a back-up proxy in the event the primary proxy is unavailable.
Religious beliefs.
Health care proxy forms are available from state websites and many hospitals have them, too. They do not require lawyers or notaries, but they must be signed by witnesses.
Example of Massachusetts Health Care Proxy form.
Example of Texas Medical Power of Attorney form.
Example of California Advanced Care Directive Form.
Medicare provides useful information and links for understanding advanced directives.
When it comes to end of life care, it’s possible that other supports may need of be put in place. Senior Solutions outlines some of the options.
Common Conditions

Migraine Headaches
Migraine headaches are more common among autistic adults than the general population.
There many kinds of headaches, and migraine headaches are much more common among autistic adults (42%) than the general population (10%). As with the general population, females are three times more likely than males to experience migraines, so autistic females are especially prone to these types of headaches.
As noted in our article on pain, it can be difficult for nonverbal adults to communicate when they have a headache and what types of symptoms they are experiencing. Some signs of migraine in autistic adults can include:
changes in eating habits
nausea or vomiting
sudden need to be in a dark space (photophobia)
sudden need to be in a quiet space (phonophobia)
repeated touching or banging of the head
eye movement or problems that indicate aura (tunnel vision, blind or color spots)
Treatment for headaches can vary depending on the kind of headache and any other medications or supplements currently prescribed. Always consult with all prescribing clinicians when considering prescription migraine medication or nutritional supplements.
The American Migraine Foundation has advice for managing migraines, including:
Eat small, balanced meals at regular intervals and avoid getting too hungry
Keep a regular sleep and exercise schedule
Limit intake of processed or fried foods, chocolate, artificial sweeteners and foods with nitrates and nitrites (check the labels on bacon, hot dogs, and other cured meats)
Avoid or limit caffeine and alcohol (especially red wine and beer)
Keep a food diary to identify foods that might trigger migraines
Harvard Health Publishing also offers specific advice on managing headaches:
5 Migraine Questions Answered
When headaches won’t go away
Older women and migraine with aura
Which migraine medications are most helpful?

Anxiety & Depression
Anxiety and depression are common in autism but may appear different from neurotypical adults.
Anxiety and depression are common among autistic adults, but may look different
About 70% of autistic people suffer from some form of anxiety, which can occur at any age. Anxiety disorders can include generalized anxiety disorder, panic disorder, social anxiety disorder, and phobia-related disorders. Autistic people are four times more likely to experience depression during their lifetime than the general population. Signs and symptoms of anxiety and depression in both neurotypical and autistic patients include:
Anxiety
Feeling nervous, restless or tense
Having a sense of impending danger, panic or doom
Having an increased heart rate (tachycardia)
Breathing rapidly (hyperventilation)
Sweating
Trembling
Feeling weak or tired
Trouble concentrating or thinking about anything other than the present worry
Having trouble sleeping
Experiencing gastrointestinal (GI) problems
Having difficulty controlling worry
Having the urge to avoid things that trigger anxiety
Depression
Feelings of sadness, tearfulness, emptiness or hopelessness
Angry outbursts, irritability or frustration, even over small matters
Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
Sleep disturbances, including insomnia or sleeping too much
Tiredness and lack of energy, so even small tasks take extra effort
Reduced appetite and weight loss or increased cravings for food and weight gain
Anxiety, agitation or restlessness
While anxiety in autistic individuals is frequently heightened by change, especially changes in routine or anticipation of new situations or expectations, the symptoms often present differently than in neurotypical patients. Sometimes anxiety that is expressed through behavior changes in autistic adults is attributed to other factors or grouped with “typical” autistic symptoms. Anxiety in patients with more severe language and cognitive impairments can be even harder to distinguish.
Some of the common manifestations of anxiety in autistic adults can include:
Social awkwardness and reluctance to engage in relationships or group activities
Perseverating on small worries, often manifested by repetitive questioning
Increases in stereotypy or repetitive behaviors (stimming)
Excessive adherence to rituals or routines
Negative thoughts, especially in children and young adults
Skin and/or nail picking
Pacing, escaping or running away
Meltdowns or tantrums
Depression can present in some more typical ways, such as excessive sleeping, loss of interest in preferred activities, and poor attention to self-care.
Autistic adults and caregivers should be aware of signs and symptoms of anxiety and depression and report them to their PCP and/or mental health provider. Because behaviors that appear to be anxiety-related can also be symptoms of various medical conditions it’s important to be proactive so that both the source of the anxiety and its underlying cause can be identified, whenever possible.
Drs. Chris McDougle and Robyn Thom are psychiatrists who specialize in treating autistic patients. They offer advice on recognizing depression in autistic adolescents in a Harvard Health article, “How can you support your teenager with autism spectrum disorder if they are depressed?”, and the suggestions they offer can also be applied to adults.
Therapeutic Treatment for anxiety and depression
Self-advocates and autistic people who feel comfortable sharing their feelings can benefit from talk therapy. It’s important to consider the best strategy for understanding and treating anxiety or depression according to the needs of the autistic person. Some approaches to treating anxiety and depression include cognitive behavioral therapy (CBT), mindfulness therapy, dialectic behavioral therapy (DBT), and neurofeedback.
Medication Treatment for anxiety and depression
Medication and autism is a complex topic. Prescription, over the counter, and complementary medications don’t always work for all patients and side effects can affect long-term health. Clinicians who treat autistic patients often find that medications and dosages that work well for neurotypical patients are less effective for those with autism. It’s important to discuss medication strategies with the PCP or any prescribing clinician to ensure that any psychotropic medications are tailored specifically to the unique needs of the autistic patient.
For example, Selective Serotonin Reuptake Inhibitors (SSRIs) are often used as a first line medication for anxiety in neurotypical patients. However, some experts in the autism field caution against their use in autistic patients, especially children and adolescents. Buspirone and mirtazapine in very small doses to start have been shown to help anxiety, with slow and steady dosing up to a typical amount.
Harvard Medical School’s free Clinician Course for medical providers, Clinical Care for Autistic Adults, provides clear and extensive advice to medical providers about best practices for treating autistic adults, including specific guidelines for medication.
Another useful resource is the Parent’s Medication Guide from the American Psychiatric Association
Suicide risk
Any language or behavior that presents a risk of serious self-harm or suicide should be reported immediately to a mental health professional or PCP. They can offer instructions about the best way to access emergency mental health services to get immediate attention.
The Suicide Hotline can be reached by calling or texting 988 from any phone. They have resources specifically designed to meet the needs of neurodiverse and autistic people:
Warning signs of suicide for autistic people
Crisis supports for the autistic community
Spark for Autism explores the risk of suicide in autistic people.
Finding Treatment for anxiety and depression
ECHO Autism has a directory for finding clinicians trained in best practices for treating autistic children and adults.
Psychology Today has an excellent directory for finding therapists, many of whom provide autism-competent care.
The AASPIRE Toolkit is a good resource that can help patients find an adult provider who understands autism-competent care.
Pennsylvania’s Autism Services, Education, Resources and Training Collaborative (ASERT) has a resource, “Be Well, Think Well”, with tools that self-advocates and caregivers can use to help with anxiety.
The National Alliance on Mental Illness (NAMI) offers help finding mental health providers and offers links to support groups.
The Substance Abuse and Mental Health Services Administration offers 24-hour referral and support.
SAMHSA’s National Helpline800-662-HELP (4357) TTY: 800-487-4889

Digestive Issues – Pica
Pica is a condition where individuals with nutrient deficiency or some other process going on causes them to chew on or ingest non-food products.
Pica is a condition in which individuals with nutrient deficiency or some other process going on causes them to chew on or ingest non-food products. While present in the neurotypical population pica does appear more often in autistic people. It’s more common in children but pica does appear in adults, particularly those who have had pica as children – it doesn’t always go away.
Sensory-seeking children and adults will sometimes chew on something as a way of meeting a sensory need and then end up swallowing part of the item. Picking at skin, fingernails, threads or fabric can be signs of anxiety and can lead to ingesting those items. Sometimes autistic people can mistake non-food items for food (mistaking a colorful eraser for a gummy bear) and eat them (even if they taste terrible).
Often a non-food item will pass through the digestive system without causing any physical harm, but toxicity or ingestion of small things over time can create significant health problems. Dr. Tim Buie, a Pediatric Gastroenterologist at Boston Children’s Hospital experience in treating autistic patients, explains:
What you worry about is what you don’t see. Individuals who might be chewing their hair or eating their hair can develop a collection of that hair and develop an intestinal obstruction. Or they’re shredding paper or they’re shredding clothing, and you think that’s just an external behavior. But then they’re imbibing that product and they’re getting intestinal symptoms or intestinal obstruction because they’ve eaten those products.
Autistic adults who exhibited pica as children should continue to be monitored for those behaviors, especially when they are under stress. That monitoring should include toileting behaviors, as rectal itching can be a sign that non-food items are being digested.
Here’s an example of a tablet device cover where the vinyl coating became loose at the edge and it was picked away and ingested by an autistic adult.
A black tablet device cover with part of the cover picked away.

Dietary Concerns
Documented food allergies are twice as common in children and adolescents with autism (10%-16%) compared to their neurotypical peers. Due to this prevalence, it’s possible that there are autistic adults...
Documented food allergies are twice as common in children and adolescents with autism (10%-16%) compared to their neurotypical peers. Due to this prevalence, it’s possible that there are autistic adults with existing food allergies that might not have been diagnosed in their younger years. Autistic adults who have been classified as selective – or picky – eaters might be avoiding food that simply does not make them feel well, whether it a true allergy or a food intolerance.
Food allergy vs food intolerance
Food allergies are a function of the immune system and can be mild or life-threatening; food intolerances take place in the digestive system and can cause significant discomfort. Harvard Health explains the difference and why it matters.
If there are persistent symptom of gastrointestinal distress, it can be helpful to keep a food diary or food log to see if incidents of nausea, vomiting, itching, diarrhea, hives and constipation can be tied to certain kinds of foods.
The Centers for Disease Control has a free, downloadable example of a simple food diary that can help patients record eating habits.
Special diets
In the early 2000s, some families of autistic children experimented with specific diets (gluten-free/casein-free, specific carbohydrate) to help address physical and behavioral issues. Although some positive results were shared, in some cases, these diets caused nutritional deficiencies that may have followed patients into adulthood. As a result of his work with autistic patients with digestive issues, Dr. Tim Buie, a pediatric gastroenterologist at Boston Children’s Hospital, doesn’t recommend a specific diet for autistic persons. Rather, he concurs that tracking and understanding what foods keep someone happy and healthy play a big role in overall GI health for autistic people.
Dr. Buie explains the role of food choices and special diets in autistic patients:
Dr. Tim Buie, MD, Gastroenterologist at Boston Children’s ospital
Picky eating
Many autistic adults gravitate toward (or avoid) foods that are a certain color or texture, or they may eat the same foods, day after day, for months or even years. These preferences are not indications of food allergies, especially if there are no symptoms of discomfort. Autistic adults don’t necessarily have to eat a wide variety of foods at every meal to meet their nutritional needs. For caregivers of autistic adults, it is important to support food choices to the extent that it’s possible and practical if they are healthy and they eat a reasonably balanced diet.
Dr. Buie understands the frustration of caregivers who worry about picky eating tendencies:
You get to be picky, just like I get to decide whether I’ll eat asparagus or not. You know, I think all of us have particular food preferences where we tend to avoid them. They become a problem when they’re impacting nutrition or when they’re impacting weight or balance in some way.
Dr. Tim Buie
Children with autism are 40% more likely to be obese as adults. Research has noted this risk but has not established an underlying cause. Genes, family history, cultural background, medication and eating habits may all play a role. An important part of adult health care is discussing nutrition with a PCP as part of managing overall good health. Weight gain or weight loss from over or under eating specific foods will be part of any yearly exam discussion with a PCP (any significant weight gain or loss should always prompt an immediate appointment). Diet and weight gain are important issues to be raised with caregivers and group home providers and staffs to assure that autistic adults have balanced diets and get regular exercise.
Celiac Disease
Celiac disease is an autoimmune condition in which ingesting gluten triggers a complex inflammatory reaction. It is no more common in autistic people than in the general population, but it is now more frequently recognized in all patients. Symptoms of celiac disease include:
Diarrhea
Weight loss or inability to gain weight
An increase in abdominal discomfort
If these symptoms exist or there’s a family history of celiac disease, a gastroenterologist can test for it through a blood test or biopsy.

Abdominal Pain
Abdominal pain can be a frequent concern throughout the lifespan of autistic people. A diagnosis can be challenging, especially for nonverbal adults, or those with limited communication skills who may have difficulty identifying and communicating the source of their pain.
Dr. Tim Buie, a pediatric gastroenterologist at Boston Children’s Hospital, notes that his nonverbal autistic patients communicate digestive discomfort in a number of ways, including:
self-biting and mouthing behaviors
chewing clothes (often sleeves), paper or other objects
ingesting nonfood items (pica)
aggression against others
twisting of the midsection or rubbing the abdomen against furniture
rubbing or scratching of the neck and throat areas
escaping or bolting
an increase in repetitive behaviors or vocalizations.
Collecting data to help locate the cause of pain
It’s important to note that GI issues are not always the culprit in digestive discomfort situations. Other pain-related behaviors could be caused by dental issues, migraine headaches, or other kinds of physical distress. Collecting data on toileting and food intake behaviors, as well as other GI-related activities, can help the clinician pinpoint what might be causing pain. See our article more information on communicating about pain.
Clinicians have found that when patients who exhibit aggression and/or self-injury are evaluated and found to have underlying GI distress, the treatment of that condition usually results in an improvement in behavior. In this video, Dr. Buie explains some of the behaviors that may indicate digestive upset:
Dr. Tim Buie, Gastroenterologist at Boston Children’s Hospital, on signs of gastrointestinal distress in autistic adults
Bowel movements
Tracking bowel movements can be helpful, as abdominal pain may occur at certain times during the digestive process. The Bristol stool chart, which helps document the timing and outcome in bowel movements, is an easy-to-use tracking tool.
Food intake
Sometimes certain foods can cause abdominal pain because they are hard to digest. Fried or spicy foods, dairy products, or vegetables such as spinach, broccoli, and cabbage can all cause discomfort. The Centers for Disease Control has a free, downloadable simple food diary that can help patients record eating habits to identify any potential problem foods or ingredients.
Warning signs of something more serious
The sudden onset of abdominal pain may indicate something more serious than digestive upset. Pain can that appears to be located on the right side of the lower abdomen or the lower back that is accompanied by nausea, loss of appetite, or fever requires immediate medical attention. Such pain could indicate appendicitis, kidney stones, diverticulitis, or another condition that requires prompt specialized care.
Although GI symptoms are common in adults, there is no single set of signs, symptoms, or treatments that applies to all autistic patients. AAHR has articles on the most common GI conditions:
GERD and acid reflux
Constipation
Pica

Gastroesophageal Reflux Disease (GERD) and Acid Reflux
Gastrointestinal problems occur two to three times more often in autistic people than in the general population.
Gastroesophageal Reflux Disease (GERD) is common in both autistic children and adults, and can affect appetite, sleep, and behavior.
Reflux is the backward flow of acid from the stomach into the esophagus. GERD is when the closure of the lower esophagus becomes weak from recurring acid reflux. Symptoms include heartburn, regurgitation, chest pain, dry cough, shortness of breath, or trouble swallowing. Persistent GERD can lead to more serious health conditions like esophagitis.
Dr. Timothy Buie, a pediatric gastroenterologist at Boston Children’s Hospital whose research and practice focuses largely on autistic patients with digestive issues, notes that non-verbal autistic people sometimes exhibit behaviors that indicate GERD, reflux, or other digestive issues. In this video, Dr. Buie explains some of the behaviors that may indicate digestive upset:
Dr. Tim Buie, Gastroenterologist at Boston Children’s Hospital, on signs of gastrointestinal distress in autistic adults
If frequent heartburn or reflux is suspected it should be brought to the attention of a PCP. They may recommend over the counter remedies such as antacids, famotidine, or omeprazole. Regardless, any condition that persists should be referred to a gastroenterologist for proper assessment, diagnosis and treatment.
Autistic adults requiring treatment for GERD may need to have an endoscopy, which is a process in which a gastroenterologist examines the digestive tract by inserting a tube with a tiny light and a camera down the throat. Because medical procedures of this kind can be particularly stressful for autistic people, patients and caregivers should discuss accommodations for making the procedure as tolerable as possible with the gastroenterologist and hospital staff. [link to accommodations article]
Dietary and Lifestyle changes to help ease reflux/GERD
Diet can contribute to the occurrence of increase stomach acid. To reduce the occurrence and uncomfortable symptoms of reflux/GERD, autistic adults will want to limit certain foods, including:
mint
orange/grapefruit juice
tomatoes
onions
chocolate
fried/spicy foods
carbonated drinks
Foods and ingredients that can help:
banana
rice
oatmeal
melon
ginger
salmon
sweet potatoes
carrots
beets
Lifestyle changes to consider:
avoid eating near bedtime
drink plenty of water
eat several small meals instead of three large ones
placing a bolster under a mattress or using extra pillows to keep the head raised, which lessens the chance of acid rising to irritate the esophagus during sleep
For autistic adults in day programs or who live in residential placements, communication about dietary health can assist in managing GI conditions. Our Dietary Plan Tool is one way of helping caregivers and staff understand and contribute to positive health across the lifespan.
A tool for tracking bowel movements when abdominal pain is a problem

Common Gastrointestinal Conditions
Autistic people are more likely to suffer from gastrointestinal (GI) ailments than the general population. They are especially more difficult to identify and diagnose in adults with communication challenges. GI...
Autistic people are more likely to suffer from gastrointestinal (GI) ailments than the general population. They are especially more difficult to identify and diagnose in adults with communication challenges. GI symptoms can range from mild stomachaches to serious, persistent vomiting. There is no single set of signs, symptoms, or treatments that applies to all autistic patients.
AAHR has articles on the most common GI conditions:
abdominal pain
constipation
GERD and acid reflux
Seeking care
Although GI symptoms are common, no digestive condition should be accepted as simply part of being autistic. It’s important that GI symptoms are addressed by a PCP or gastroenterologist to avoid serious health consequences during the adult years.
An adult patient who has been under the care of a pediatric gastroenterologist for ongoing digestive issues should transfer their care to an adult gastroenterologist. Communicating about the symptoms, how they present, and how they’ve been treated — through diet and/or medication — is important to assuring good health over the lifespan.
Behavior as communication about pain
Caregivers should note that behaviors of all kinds are a form of communication, and sometimes that communication is speaking about pain. Aggression and self-injury are not core symptoms of autism. When such behaviors do appear, it’s important to consider whether they indicate that an autistic adult is in pain. Gastrointestinal problems often create the kind of discomfort that can lead to behaviors (or an increase in the kinds of behaviors) that are core signs and symptoms of autism. Examples of behaviors that may indicate pain are:
self-biting and mouthing behaviors
chewing clothes (often sleeves), paper, or other objects
ingesting nonfood items (pica)
aggression against others
twisting of the midsection or rubbing the abdomen against furniture
rubbing or scratching neck or throat areas
escaping or bolting
an increase in repetitive behaviors or vocalizations.
Autistic adults or caregivers should record when, where, and how often these behaviors occur, in preparation for discussing them with a PCP or gastroenterologist so that a full diagnosis can be made. If the underlying cause turns out to be GI distress, treatment of that condition very often results in an improvement in the behavior(s). AAHR has more information on communicating about pain.
Keep in mind that GI issues are not always the culprit. Mental health issues such as anxiety can also trigger GI symptoms, and other pain-related behaviors could be caused by dental issues, migraine headaches, or other kinds of physical distress. Each of these possibilities can be discussed with a PCP, who can then make referrals to one or more specialists.
We recognize that gastrointestinal problems are very common in the population of individuals with autism. And that’s true at all ages, from childhood to adulthood. The frequency of GI issues in individuals with autism is greater than the general population. It’s perhaps 2 to 3 times more frequent to see gastrointestinal problems in this population than the general population.
Dr. Tim Buie, Pediatric Gastroenterologist, Boston Children’s Hospital

Constipation
This most common of complaints for autistic people may require consulting a gastroenterologist and a nutritionist.
Constipation is the most common gastrointestinal complaint in autistic people as well as in the general population. For many people, constipation is a chronic health problem that can develop and persist at any point in the lifespan.
Signs of constipation include:
three or fewer bowel movements a week
lumpy or hard stools
pain during bowel movements
difficulty completely emptying the bowel.
Symptoms of constipation can present differently in autistic people, especially those with more severe language and cognitive impairments. For example, contorting the body in unusual ways can indicate abdominal pain. Dr. Tim Buie, a pediatric gastroenterologist at Boston Children’s Hospital, notes that his autistic patients sometime exhibit “behaviors such as pressing their bellies onto a chair, leaning onto furniture, or lying flat on their bellies to kind of seek pressure on their bellies. That’s a common thing that people have associated with constipation.” These behaviors may indicate the need to consult a gastroenterologist. In this video, Dr. Buie explains some of the behaviors that may indicate digestive upset:
Dr. Tim Buie, Gastroenterologist at Boston Children’s Hospital, on signs of gastrointestinal distress in autistic adults
Functional fecal retention (FFR)
Functional fecal retention (FFR) is a gastrological condition that appears frequently in autistic people. It is characterized by more regularly occurring stools but with less complete evacuation. Because the bowel is never completely empty, even with regular toileting occurrences, symptoms such as abdominal pain, bloating, or toileting accidents caused by a loss of control of the pelvic floor muscles can develop. Anxiety, sensory, or attention issues can contribute to the development of FFR. Note that anxiety might not initially be directly related to toileting issues, but if constipation persists it can itself become a source of anxiety and lead to FFR.
Tracking toileting patterns
In addition to caregivers, personal care attendants and group home staff can provide feedback on any patterns such as constipation, FFR, soiling, withholding, or not using the toilet often enough. Tracking toileting behaviors and characteristics of bowel movement can help provide much needed detail for the PCP or gastroenterologist. The Bristol Stool Chart is a useful tool specifically for tracking bowel movements. Caregivers and autistic patients can record data and look for patterns that, in consultation with a PCP or gastroenterologist, can identify and address sources of constipation.
Lifestyle changes to help ease constipation
Diet and certain medications can contribute to chronic constipation. Autistic adults will want to have regular conversations with a gastroenterologist (and possibly a nutritionist) to determine the underlying causes and best approaches for managing it. Caregivers are advised to take cues from the autistic adult’s clinician and avoid making diet, food, or exercise into battleground issues, as stress and anxiety can lead to or exacerbate bowel issues.
Lifestyle changes that may be helpful for constipation include staying hydrated by drinking plenty of water and eating foods that are rich in water and/or fiber. Keep in mind that adjustments in diet should be approached slowly; adding or eliminating one kind of food at a time will make it easier to measure the impact of the change. A nutritionist can provide more tailored recommendations for autistic adults; however, some general examples of foods to help alleviate constipation include:
whole-grain breads
oatmeal
beans and chickpeas
veggies: carrots, broccoli, peas, and collard greens
nuts: peanuts, almonds, and pecans
fruit: berries, apples, and pears
High-fat foods tend to be low in fiber and can slow down digestion. Foods that are high in processed sugar, salt, and/or fat content, and low in water, can contribute to chronic constipation. Limit or avoid foods such as:
fast food, such as french fries and chicken nuggets
processed meats with nitrates like hot dogs and sausages
salty snack foods
Regular exercise helps stimulate bowel movement, so daily movement such as walking or swimming can help with chronic constipation. Frequent use of over-the-counter laxatives should be avoided.
For those in day programs or who live in residential placements, communication about dietary health can assist in managing conditions like constipation. Our Dietary Plan Tool is one way of helping caregivers and staff understand and maintain good health in autistic adults.
Health Care Plan Template for communicating about current health and dietary needs and interventions.

Sleep Problems
Sleep problems are common in autistic people. As many as 50-80% experience some kind of sleep difficulty as compared to 25-30% of neurotypical people.
Sleep problems are common in autistic people. As many as 50-80% experience some kind of sleep difficulty as compared to 25-30% of neurotypical people. Sleep issues vary widely and include:
Difficulty falling asleep
Interrupted sleep
Early waking
Needing very little sleep
When sleep problems arise in the adult years, there could be a variety of explanations, including environmental factors, changes in family or living arrangements, transitions to new day programs or employment, or environmental factors such a seasonal allergies or other air quality issues. Sleep problems can also be caused or exacerbated by underlying medical conditions such as:
Sleep apnea
GERD or acid reflux
Constipation
Seizures
Erupting wisdom teeth
Restless legs syndrome
Psychological factors and emotional distress can also contribute to sleep problems. Anxiety, depression, stress, or trauma are just a few of the factors that can create or exacerbate sleep problems. Some types of medications, such as stimulants, beta blockers, corticosteroids, and decongestants can also affect the quality and duration of nighttime sleep.
Lifestyle changes can help
Six simple things to do to improve sleep:
Increase the amount of exercise during the day, such as walking and swimming
Minimize alcohol and caffeine intake
Limit screen use at night when possible
If heartburn or acid reflux are suspected, prop up the head of the bed or use extra pillows to avoid laying completely flat on the bed
Keep the bedroom cool and as dark as possible
Consider a weighted blanket to help calm nerves and give calming sensory input
Seeking care
When simple interventions don’t help, make an appointment with a PCP. A wearable device such as a smart watch or using a phone app that tracks sleep quality and waking patterns can provide useful feedback. Based on symptoms, history, and assessment, a referral to a neurologist or mental health clinician may be recommended. If symptoms include snoring or disrupted breathing, a sleep study to rule out sleep apnea or narcolepsy can often be done at home. If an overnight sleep study is required, there are accommodations than can make these studies less stressful. The Vanderbilt Kennedy Center has a guide for helping children with sleep study protocol that is also useful for adults.
Resources for sleep issues
Learn more about sleep and autism, and the impact of sleep patterns on other conditions common in older adults:
Spectrum News discusses the latest sleep research in Cracking Sleep’s Conundrum
Harvard Health Publishing on Sleep Problems and Risk of Stroke
Harvard Health Publishing on sleep problems and the increased risk of cardiovascular disease
Healthy Sleep Tips from the Harvard Division of Sleep Medicine
Sleep Strategies for Teens with Autism Spectrum Disorder from the Vanderbilt Kennedy Center and Autism Speaks
Weighted blankets can promote better sleep.

Common Medical Conditions in Autistic Adults – An Overview
Understanding some of the common medical conditions that occur in autistic adults is a key part of managing medical care.
Health needs change for everyone as they get older and it’s no different for autistic people, but understanding and approaching the aging process can look a little different for autistic adults. Some medical conditions occur more frequently in autistic people and they may also present differently than in their neurotypical people. Medical conditions may often appear in childhood while others might only emerge later in life. They often occur jointly with other health conditions and are often referred to as “co-occuring” or “co-morbid” conditions.
Mental health conditions
Mental health issues are common in people with autism, with up to 80% experiencing some mental health condition. They can include:
ADHD (attention deficit hyperactivity disorder)
Anxiety
Depression
Irritability
Physical conditions
Many physical conditions, including heart and lung conditions and diabetes, are more common in adults with autism. Other common physical conditions may include:
Neurological issues
Migraine headaches
Seizures
Sleep problems
Stomach and digestive problems
Constipation
Acid reflux (GERD)
Dietary issues (food allergies and intolerances)
Pica
Abdominal pain

Attention Deficit Hyperactivity Disorder (ADHD)
Dr. Chris McDougle, a psychiatrist who is the Director of Lurie Center for Autism, notes that “ADHD is very common in children with autism. And like in regular ADHD, the...
Dr. Chris McDougle, a psychiatrist who is the Director of Lurie Center for Autism, notes that “ADHD is very common in children with autism. And like in regular ADHD, the hyperactivity and impulsivity can lessen over time when you get into teenagers or early adult years. But the inattention can persist.”
Some of the signs of ADHD in autistic adults are:
Hyperactivity
Impulsivity
Inattention
Problems with organization or executive function
Medication
Many patients with ADHD benefit from medication but experts like Dr. McDougle indicate that autistic patients respond differently to medication than their neurotypical peers.
Harvard Medical School’s free Clinician Course for medical providers, Clinical Care for Autistic Adults, provides clear and extensive advice to medical providers about best practices for treating autistic adults, including specific guidelines for medication.
Additional content in development September 2023
Staying Healthy

Dietary Plan Tool for Schools and Day Programs
Autistic adults with special dietary needs and behaviors around food can benefit from a form that outlines those needs and the best interventions for use at school or day programs.
Autistic adults with special dietary needs and behaviors around food can benefit from a form that outlines those needs and the best interventions for use at school or day programs. Many school districts have a similar form for the school nurse but that information doesn’t always follow the adult after they turn 22.
We’ve designed an easy-to-use template based on the dietary information school districts require.

Dietary Concerns
Documented food allergies are twice as common in children and adolescents with autism (10%-16%) compared to their neurotypical peers. Due to this prevalence, it’s possible that there are autistic adults...
Documented food allergies are twice as common in children and adolescents with autism (10%-16%) compared to their neurotypical peers. Due to this prevalence, it’s possible that there are autistic adults with existing food allergies that might not have been diagnosed in their younger years. Autistic adults who have been classified as selective – or picky – eaters might be avoiding food that simply does not make them feel well, whether it a true allergy or a food intolerance.
Food allergy vs food intolerance
Food allergies are a function of the immune system and can be mild or life-threatening; food intolerances take place in the digestive system and can cause significant discomfort. Harvard Health explains the difference and why it matters.
If there are persistent symptom of gastrointestinal distress, it can be helpful to keep a food diary or food log to see if incidents of nausea, vomiting, itching, diarrhea, hives and constipation can be tied to certain kinds of foods.
The Centers for Disease Control has a free, downloadable example of a simple food diary that can help patients record eating habits.
Special diets
In the early 2000s, some families of autistic children experimented with specific diets (gluten-free/casein-free, specific carbohydrate) to help address physical and behavioral issues. Although some positive results were shared, in some cases, these diets caused nutritional deficiencies that may have followed patients into adulthood. As a result of his work with autistic patients with digestive issues, Dr. Tim Buie, a pediatric gastroenterologist at Boston Children’s Hospital, doesn’t recommend a specific diet for autistic persons. Rather, he concurs that tracking and understanding what foods keep someone happy and healthy play a big role in overall GI health for autistic people.
Dr. Buie explains the role of food choices and special diets in autistic patients:
Dr. Tim Buie, MD, Gastroenterologist at Boston Children’s ospital
Picky eating
Many autistic adults gravitate toward (or avoid) foods that are a certain color or texture, or they may eat the same foods, day after day, for months or even years. These preferences are not indications of food allergies, especially if there are no symptoms of discomfort. Autistic adults don’t necessarily have to eat a wide variety of foods at every meal to meet their nutritional needs. For caregivers of autistic adults, it is important to support food choices to the extent that it’s possible and practical if they are healthy and they eat a reasonably balanced diet.
Dr. Buie understands the frustration of caregivers who worry about picky eating tendencies:
You get to be picky, just like I get to decide whether I’ll eat asparagus or not. You know, I think all of us have particular food preferences where we tend to avoid them. They become a problem when they’re impacting nutrition or when they’re impacting weight or balance in some way.
Dr. Tim Buie
Children with autism are 40% more likely to be obese as adults. Research has noted this risk but has not established an underlying cause. Genes, family history, cultural background, medication and eating habits may all play a role. An important part of adult health care is discussing nutrition with a PCP as part of managing overall good health. Weight gain or weight loss from over or under eating specific foods will be part of any yearly exam discussion with a PCP (any significant weight gain or loss should always prompt an immediate appointment). Diet and weight gain are important issues to be raised with caregivers and group home providers and staffs to assure that autistic adults have balanced diets and get regular exercise.
Celiac Disease
Celiac disease is an autoimmune condition in which ingesting gluten triggers a complex inflammatory reaction. It is no more common in autistic people than in the general population, but it is now more frequently recognized in all patients. Symptoms of celiac disease include:
Diarrhea
Weight loss or inability to gain weight
An increase in abdominal discomfort
If these symptoms exist or there’s a family history of celiac disease, a gastroenterologist can test for it through a blood test or biopsy.
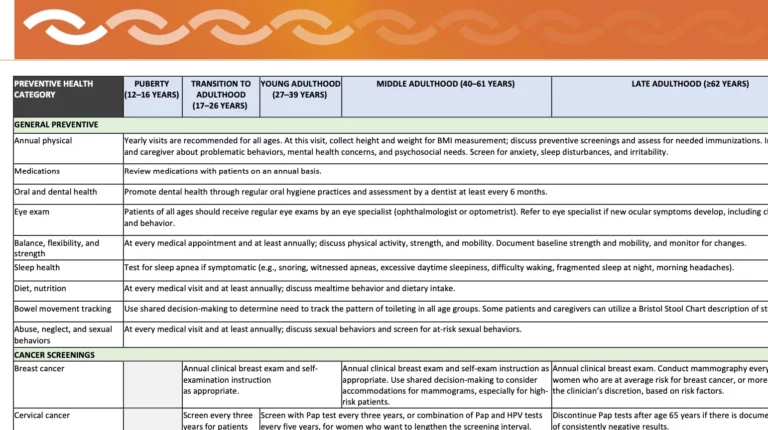
Useful Information about Preventive Care
As part of its free course, Clinical Care for Autistic Adults, Harvard Medical School developed a useful time line for preventive health care screenings and immunizations for autistic adults.
This downloadable and printable Autism Preventive Health Table was developed as part of the Harvard Medical School’s course, Clinical Care for Autistic Adults. It lists baseline preventive health care screenings and immunizations for autistic adults. The intended audience is primary care physicians but feel free to use as a reference and to share with your PCPs or other providers. Key points for caregivers and self-advocates to note:
Schedule all annual exams well in advance so that the appointment happens at a time of year and time of day that works best for the patient/family.
If possible, gather information about health conditions that can run in families such as heart problems, cancer, diabetes, depression, and addiction. This information can help identify the most important screenings and how often they should be done.
A guide to share with providers for preventive health care
The information on the table is based on the following sources:
Adult Immunization Schedule by Age, CDC, 2023.
CDC: Cancer Screening Tests. Accessed on April 1, 2023.
Dhanasekara CS, Ancona D, Cortes L, et al. Association Between Autism Spectrum Disorders and Cardiometabolic Diseases: A Systematic Review and Meta-analysis. JAMA Pediatr. 2023;177(3):248-257. doi:10.1001/jamapediatrics.2022.5629
Isenberg BM, Yule AM, McKowen JW, Nowinski LA, Forchelli GA, Wilens TE. Considerations for Treating Young People With Comorbid Autism Spectrum Disorder and Substance Use Disorder. J Am Acad Child Adolesc Psychiatry. 2019;58(12):1139-1141. doi:10.1016/j.jaac.2019.08.467
Massachusetts Department of Developmental Services Adult Screening Recommendations 2019, Mass.gov.Accessed on April 1, 2023.
Schick, Elizabeth, Is It Safe to Sedate our Son at the Dentist? Autism Speaks. 2014. Accessed on April 1, 2023.
Screening and Preventive Interventions for Oral Health in Children 5 Years and Older and Adults, U.S. Preventive Services Task Force. Accessed on April 1, 2023.
Sexually Transmitted Infections Treatment Guidelines, 2021, CDC. Accessed on April 1, 2023.
Dr. James Bath, a primary care physician for autistic adults at the MGH Lurie Center for Autism, discusses the importance of preventive care as key to a long, healthy life:
Dr. James Bath, Adult Primary Care Physician at the MGH Lurie Center for Autism







